Introduction to the Pediatric Chain of Survival
In the realm of emergency medical care, particularly concerning pediatric patients, the concept of the Pediatric Chain of Survival stands as a critical framework. This paradigm outlines a series of essential steps aimed at optimizing outcomes for children experiencing sudden cardiac arrest or other life-threatening emergencies. Just as in adults, timely and effective interventions are paramount in saving lives among the pediatric population.
A profound understanding of the Pediatric Chain of Survival is indispensable for healthcare providers, caregivers, and anyone involved in the care of children. From recognizing the initial signs of distress to delivering advanced life support interventions, each link in the chain plays a crucial role in the survival journey of a pediatric patient.
Initial Recognition and Activation
The first link in the Pediatric Chain of Survival emphasizes the importance of prompt recognition and activation of the emergency response system. In pediatric emergencies, swift identification of distress signals is vital for initiating appropriate interventions. Caregivers, parents, teachers, and healthcare providers must be equipped with the knowledge to recognize signs of potentially life-threatening situations in children, such as respiratory distress, altered mental status, or sudden collapse.
Upon recognizing these signs, activating the emergency response system without delay is imperative. Time is of the essence in pediatric emergencies, and every moment counts towards initiating life-saving measures. Whether it’s calling 911 or initiating an in-house emergency response protocol, the swift activation of the appropriate channels ensures that help is on the way without delay.
Early CPR
As we delve deeper into the Pediatric Chain of Survival, the significance of early CPR emerges as a cornerstone in the cascade of interventions aimed at saving the lives of pediatric patients. CPR, or Cardiopulmonary Resuscitation, is a life-saving technique that combines chest compressions and rescue breaths to maintain blood flow and oxygenation to vital organs during cardiac arrest.
In pediatric emergencies, prompt initiation of CPR can mean the difference between life and death. Children experiencing cardiac arrest often have underlying causes such as respiratory failure, drowning, or sudden cardiac events. Effective CPR buys precious time for the arrival of advanced medical care and increases the likelihood of a positive outcome.
Here are key points to consider regarding early CPR in the context of pediatric emergencies:
- Importance of Early CPR: Time is critical in pediatric cardiac arrest situations. Early CPR helps to maintain circulation and oxygenation to the brain and other vital organs, significantly improving the chances of survival.
- Techniques for Performing Pediatric CPR: CPR techniques for children differ from those used for adults. Proper hand placement, compression depth, and rate are essential for effective chest compressions in pediatric patients. Additionally, rescue breaths should be administered in a manner appropriate for the child’s age and size.
- Training and Certification: Healthcare providers and caregivers should undergo regular training and certification in pediatric CPR to ensure competency in performing life-saving interventions. CPR Cincinnati offers comprehensive courses that cover pediatric CPR techniques in depth, providing participants with the skills and confidence to respond effectively to pediatric emergencies.
By emphasizing the importance of early CPR and providing training opportunities for healthcare providers and caregivers, we can strengthen the Pediatric Chain of Survival and improve outcomes for pediatric patients in critical situations.
Early Access to the Emergency Medical Services (EMS) System
After the initiation of early CPR, the next crucial link in the Pediatric Chain of Survival is early access to the emergency medical services (EMS) system. While CPR provides immediate intervention to maintain blood flow and oxygenation, access to advanced medical care is essential for the successful resuscitation and stabilization of pediatric patients.
Here’s why early access to the EMS system is pivotal in pediatric emergencies:
- Advanced Medical Care: EMS providers are trained to deliver advanced medical interventions, including advanced airway management, medication administration, and defibrillation. These interventions are often necessary to restore normal cardiac rhythm and address underlying causes of cardiac arrest in pediatric patients.
- Timely Response: EMS systems are equipped to respond rapidly to pediatric emergencies, with specialized pediatric equipment and protocols in place to address the unique needs of children. The prompt arrival of EMS providers ensures that advanced medical care is initiated without delay, optimizing outcomes for pediatric patients.
- Coordination of Care: EMS providers play a crucial role in coordinating care between pre-hospital and hospital settings. They communicate vital information about the patient’s condition and treatment provided en route to the hospital, facilitating a seamless transition of care upon arrival.
Collaboration between bystanders, healthcare providers, and EMS personnel is essential to ensure timely access to advanced medical care for pediatric patients in critical situations. CPR Cincinnati emphasizes the importance of activating the EMS system early in pediatric emergencies and provides training to equip healthcare providers and caregivers with the knowledge and skills to do so effectively.
Pediatric Advanced Life Support (PALS)
Pediatric Advanced Life Support (PALS) represents a critical component of the Pediatric Chain of Survival, focusing on advanced interventions and protocols specifically tailored to manage pediatric cardiac arrest and other life-threatening emergencies. PALS guidelines are developed by organizations such as the American Heart Association (AHA) to provide evidence-based recommendations for healthcare providers caring for pediatric patients in acute settings.
Key aspects of Pediatric Advanced Life Support include:
- Advanced Interventions: PALS encompasses a range of advanced interventions tailored to the unique physiological and anatomical characteristics of pediatric patients. These interventions may include advanced airway management, intravenous medication administration, and synchronized cardioversion for unstable arrhythmias.
- Team-Based Approach: PALS emphasizes a team-based approach to pediatric resuscitation, recognizing the importance of effective communication, leadership, and coordination among healthcare providers. Team dynamics play a crucial role in optimizing the delivery of care and maximizing the chances of a positive outcome for pediatric patients.
- Simulation-Based Training: Effective PALS training often incorporates simulation-based scenarios that replicate real-life pediatric emergencies. This hands-on approach allows healthcare providers to practice clinical skills, decision-making, and teamwork in a controlled environment, enhancing readiness to respond to actual emergencies.
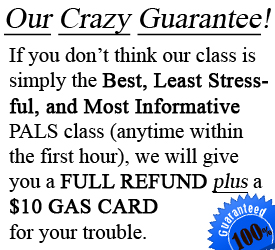
At CPR Cincinnati, we offer comprehensive PALS training courses designed to equip healthcare providers with the knowledge and skills necessary to effectively manage pediatric emergencies. Our experienced instructors provide hands-on training and simulation scenarios that simulate real-world pediatric resuscitation situations, ensuring that participants feel confident and prepared to respond when faced with a pediatric patient in distress.
Integrated Post-Cardiac Arrest Care
While successful resuscitation marks a critical milestone in the Pediatric Chain of Survival, the journey toward optimal recovery continues with integrated post-cardiac arrest care. Integrated post-cardiac arrest care involves a comprehensive and coordinated approach to managing pediatric patients following resuscitation, focusing on stabilizing physiological functions, identifying and addressing underlying causes, and supporting neurological recovery.
Key components of integrated post-cardiac arrest care include:
- Neurological Monitoring: Following resuscitation from cardiac arrest, pediatric patients require close neurological monitoring to assess brain function and detect any signs of neurological injury. Continuous assessment of consciousness, pupil reactivity, and neurological reflexes helps guide treatment decisions and prognostication.
- Targeted Temperature Management: Targeted temperature management, also known as therapeutic hypothermia or controlled normothermia, may be employed in pediatric patients following cardiac arrest to mitigate neurological injury and improve outcomes. This intervention involves carefully regulating the patient’s body temperature within a specific range for a defined duration.
- Multidisciplinary Support: Integrated post-cardiac arrest care involves collaboration among a multidisciplinary team of healthcare providers, including critical care physicians, neurologists, cardiologists, nurses, and rehabilitation specialists. Each member of the team plays a vital role in optimizing the patient’s recovery and long-term outcomes.
- Family-Centered Care: In addition to medical interventions, integrated post-cardiac arrest care prioritizes family-centered care, recognizing the crucial role of parents and caregivers in the patient’s recovery journey. Open communication, emotional support, and involvement in decision-making empower families to participate actively in the care process.
By implementing a comprehensive and coordinated approach to post-cardiac arrest care, healthcare providers can maximize the chances of a positive outcome for pediatric patients following resuscitation. CPR Cincinnati emphasizes the importance of ongoing training and education in integrated post-cardiac arrest care, equipping healthcare providers with the knowledge and skills necessary to provide optimal care to pediatric patients in critical situations.
Conclusion:
In the realm of pediatric emergency medicine, the Pediatric Chain of Survival serves as a guiding framework, outlining essential steps to optimize outcomes for children experiencing life-threatening emergencies. From early recognition and activation to integrated post-cardiac arrest care, each link in the chain plays a vital role in saving lives and ensuring the best possible outcomes for pediatric patients.
At CPR Cincinnati, we are committed to equipping healthcare providers, caregivers, and community members with the knowledge and skills necessary to respond effectively to pediatric emergencies. Our American Heart Association training site offers a comprehensive range of courses, including CPR certification Cincinnati and PALS certification Cincinnati, designed to empower individuals to become confident and competent responders in critical situations.
By enrolling in CPR certification and PALS certification courses at CPR Cincinnati, you can make a difference in the lives of pediatric patients in your community. Our stress-free and hands-on classes provide practical training that prepares you to respond confidently to pediatric emergencies, whether you’re a healthcare professional, teacher, parent, or caregiver.
Don’t wait until an emergency strikes. Take action today to enhance your skills and preparedness in pediatric emergency care. Join us at CPR Cincinnati and become part of the chain of survival that saves lives and makes a difference in the lives of children.
Enroll now and experience the best CPR in Cincinnati!