During cardiac emergencies, proper compression depth can mean the difference between life and death. Healthcare providers and trained responders must understand the critical importance of maintaining accurate compression depth throughout cardiopulmonary resuscitation. This comprehensive guide explores essential techniques and indicators that ensure effective chest compressions during cardiac arrest situations.
Understanding the Fundamentals of Compression Depth
Effective CPR relies heavily on achieving the correct compression depth with each chest compression. The human heart requires adequate pressure to circulate blood effectively when natural cardiac function stops. Without proper compression depth, blood flow to vital organs becomes insufficient, reducing the chances of successful resuscitation.
Modern resuscitation science emphasizes that compression depth directly correlates with survival outcomes. Research consistently shows that deeper compressions generate better coronary perfusion pressure, which is essential for maintaining blood flow to the heart muscle itself. However, compressions that are too deep can cause serious injuries, while shallow compressions fail to generate adequate circulation.
When Performing Effective CPR: What is the Depth of Compression?
The American Heart Association guidelines specify that adult chest compressions should reach a depth of at least 2 inches (5 centimeters) but no more than 2.4 inches (6 centimeters). This compression depth range ensures optimal blood circulation while minimizing the risk of internal injuries.
For pediatric patients, compression depth varies based on age and size. Infants require compressions of at least one-third the chest depth, approximately 1.5 inches (4 centimeters). Children need compressions of at least one-third the chest depth, which typically measures about 2 inches (5 centimeters). These measurements ensure that compressions generate adequate blood flow without causing excessive trauma to developing chest structures.
Healthcare providers must remember that achieving proper compression depth requires significant physical effort. The chest wall offers considerable resistance, and effective compressions often require more force than rescuers initially expect. Training with feedback devices helps providers develop the muscle memory necessary to maintain consistent compression depth throughout prolonged resuscitation efforts.
What is the Most Accurate Indicator of Effective Heart Compressions During CPR?
Several indicators help determine whether chest compressions achieve adequate depth and effectiveness. The most reliable indicator is the use of real-time feedback devices that measure compression depth, rate, and recoil. These devices provide immediate audio and visual feedback, allowing rescuers to adjust their technique instantly.
End-tidal carbon dioxide monitoring serves as another excellent indicator of compression effectiveness. When compressions generate adequate circulation, carbon dioxide levels typically increase as blood flow improves. A sudden rise in end-tidal CO2 often indicates return of spontaneous circulation, while consistently low levels may suggest inadequate compression depth.
Arterial waveform monitoring, when available, provides direct visualization of the pressure generated by each compression. This real-time feedback allows healthcare providers to see immediately whether their compressions produce adequate pressure waves. Additionally, the presence of a palpable pulse during compressions indicates effective compression depth and technique.
Visual indicators also play important roles in assessing compression effectiveness. Proper compression depth should visibly depress the chest wall, and complete recoil between compressions is essential for venous return. Rescuers should observe the chest rising and falling with each compression cycle, ensuring that they allow complete chest wall recoil.
What’s the Correct Depth to Press Down During CPR Compression Depth?
Achieving the correct compression depth requires proper body positioning and technique. Rescuers should place the heel of one hand on the lower half of the breastbone, with the second hand positioned on top, interlocking fingers. The compression force should come from the shoulders and upper body weight, not just the arms.
The compression technique involves pushing hard and fast, allowing complete chest recoil between compressions. Rescuers should avoid leaning on the chest between compressions, as this prevents proper venous return. The compression rate should be maintained at 100 to 120 compressions per minute while consistently achieving the target depth range.
Body mechanics significantly impact the ability to maintain proper compression depth. Rescuers should position themselves directly over the patient’s chest, keeping their arms straight and shoulders aligned over their hands. This positioning allows the rescuer to use their body weight effectively while maintaining control over compression depth.
Fatigue represents a major challenge in maintaining adequate compression depth. Studies show that compression quality deteriorates significantly after just two minutes of continuous CPR. Therefore, rescuers should rotate every two minutes to ensure consistent compression depth throughout the resuscitation effort.
Advanced Techniques for Maintaining Compression Depth Accuracy
Professional healthcare environments often utilize mechanical compression devices that automatically maintain consistent compression depth and rate. These devices eliminate human fatigue factors and provide standardized compressions throughout extended resuscitation efforts. However, proper manual technique remains essential, as mechanical devices are not always available.
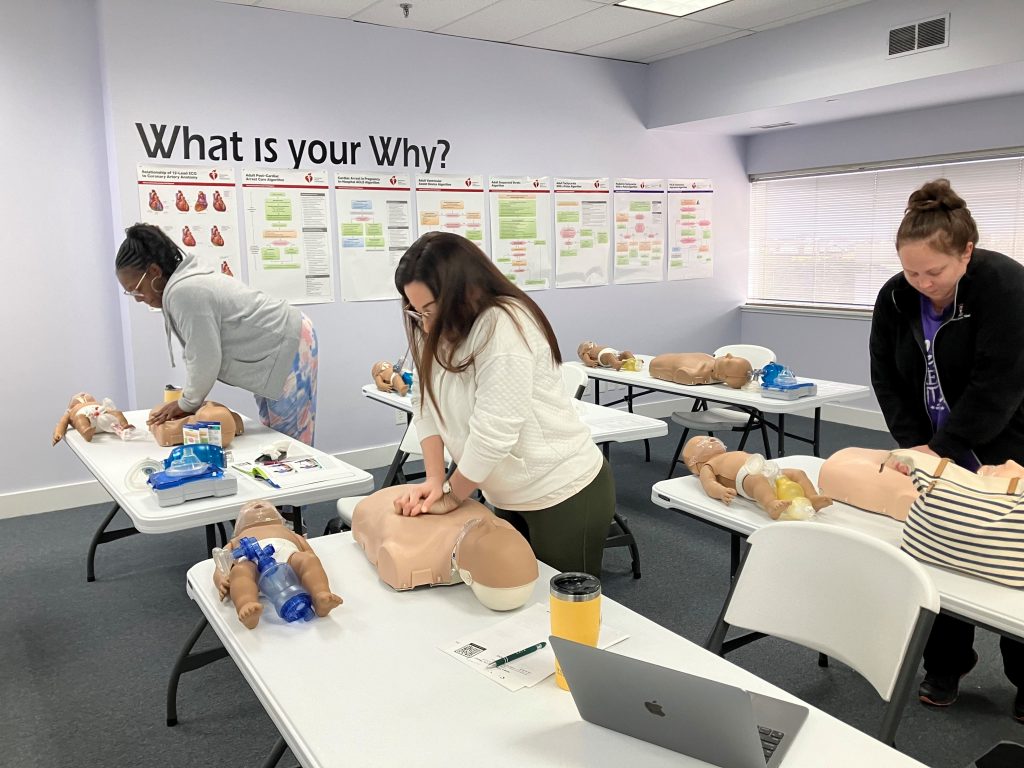
Training programs increasingly incorporate high-fidelity simulators that provide real-time feedback on compression depth, rate, and hand positioning. These simulators help healthcare providers develop muscle memory for proper compression depth while learning to recognize the tactile feedback associated with effective compressions.
Team-based approaches to CPR improve compression depth consistency. Designated team members can monitor compression quality and provide verbal feedback to the person performing compressions. This collaborative approach helps maintain high-quality compressions while allowing the primary rescuer to focus on technique.
Common Mistakes That Affect Compression Depth
Many rescuers consistently underestimate the force required to achieve adequate compression depth. The chest wall provides significant resistance, and effective compressions often feel more aggressive than rescuers expect. This psychological barrier can lead to inadvertently shallow compressions that fail to generate adequate circulation.
Incomplete chest recoil represents another common error that affects compression effectiveness. Rescuers sometimes lean on the chest between compressions or fail to allow complete chest wall return. This incomplete recoil reduces venous return and compromises the effectiveness of subsequent compressions.
Hand positioning errors can also impact compression depth effectiveness. Compressions delivered too high on the chest may not generate adequate circulation, while compressions too low risk abdominal organ injury. Proper hand placement on the lower half of the breastbone ensures optimal compression transmission to the heart.
Technology and Compression Depth Monitoring
Modern CPR feedback devices revolutionize compression depth accuracy by providing real-time guidance. These devices use accelerometers and force sensors to measure compression depth precisely, alerting rescuers when compressions are too shallow or too deep. Audio and visual feedback help rescuers maintain consistent technique throughout the resuscitation effort.
Smartphone applications now offer CPR guidance with compression depth feedback, making training more accessible. While these applications cannot replace formal training, they provide valuable practice opportunities and help maintain skill proficiency between formal training sessions.
Advanced monitoring systems in hospital settings can track compression quality metrics throughout the entire resuscitation effort. This data helps healthcare teams analyze their performance and identify areas for improvement in future cardiac arrest responses.
Conclusion: Mastering Compression Depth for Better Outcomes
Accurate compression depth remains fundamental to successful CPR outcomes. Healthcare providers and trained responders must commit to continuous practice and skill refinement to maintain proficiency in this critical skill. Understanding the correct compression depth ranges, recognizing indicators of effective compressions, and avoiding common mistakes significantly improve patient survival chances.
Regular training with feedback devices, proper body mechanics, and team-based approaches all contribute to maintaining optimal compression depth throughout cardiac arrest situations. As resuscitation science continues to evolve, staying current with guidelines and best practices ensures that rescuers provide the highest quality care possible.
Take Action: Enhance Your CPR Skills Today
Don’t wait until an emergency strikes to improve your CPR compression depth technique. Professional training provides the hands-on experience necessary to master proper compression depth and recognize effective CPR indicators.
CPR Kansas City, an American Heart Association training site, offers comprehensive certification programs that focus on proper compression depth technique. Their stress-free, hands-on classes cover BLS for Healthcare Providers, ACLS, PALS, and CPR and First Aid courses. Whether you need initial CPR certification Kansas City training, or are seeking BLS certification Kansas City for healthcare professionals, their expert instructors provide the best CPR training in the Kansas City area.
Register today for professional CPR training that emphasizes accurate compression depth techniques. Your skills could save a life, and proper training ensures you’re prepared to provide effective compressions when every second counts.