Understanding Pediatric Bag Valve Mask Ventilation
Pediatric bag valve mask ventilation represents one of the most critical skills healthcare providers must master. The American Heart Association’s 2025 guidelines emphasize that effective airway management and ventilation are fundamental components of pediatric resuscitation. Most pediatric cardiac arrests stem from respiratory deterioration or shock rather than primary cardiac events. This makes proper bag valve mask technique essential for positive patient outcomes.
Unlike adult resuscitation, where chest compressions take priority, pediatric emergencies demand equal attention to ventilation. Children experiencing respiratory failure require immediate, effective bag valve mask intervention. Understanding the unique anatomical and physiological differences in pediatric patients guides successful ventilation strategies.
Why Pediatric Bag Valve Mask Ventilation Skills Matter
Healthcare providers face unique challenges when performing bag valve mask ventilation on children. Pediatric airways differ significantly from adult airways in size, compliance, and reactivity. Recent studies demonstrate that bag valve mask ventilation, when performed correctly, can successfully manage most pediatric respiratory emergencies without requiring advanced airway placement.
The 2025 American Heart Association and American Academy of Pediatrics guidelines confirm that asphyxial cardiac arrest occurs more commonly in infants and children than ventricular fibrillation. This pattern makes ventilation extremely important during pediatric resuscitation. Research shows that combining ventilations with chest compressions produces better outcomes for asphyxial arrest than compressions alone.
However, improper technique carries serious risks. Studies published in StatPearls warn that complications from bag valve mask ventilation include barotrauma from excessive lung inflation and gastric insufflation, leading to vomiting and aspiration. Healthcare providers must balance delivering adequate tidal volumes while avoiding these dangerous complications.
Essential Components of Pediatric Bag Valve Mask Technique
Selecting the Right Equipment
Proper equipment selection forms the foundation of successful pediatric bag valve mask ventilation. Pediatric BVM devices typically contain 500-1000 mL capacity with stroke volumes of 450-650 mL, compared to adult bags holding 1500-2000 mL. Infant bags are even smaller, at approximately 240-300 mL.
The face mask must fit snugly over the child’s nose and mouth without covering the eyes. Clear masks allow providers to observe lip color and detect any regurgitation. Many pediatric BVMs include pressure-relief valves that vent at approximately 35-45 cm H₂O, helping reduce barotrauma risk from accidental over-pressurization.
Achieving Proper Head Positioning
Correct positioning opens the airway and prevents obstruction. The “sniffing position” aligns the external auditory meatus with the sternal notch. For infants, avoid hyperextension as this can actually close the airway. A small towel placed under the shoulders often helps achieve optimal alignment.
The head tilt-chin lift maneuver works for most situations. If spinal injury is suspected, use the jaw thrust technique instead. Oropharyngeal or nasopharyngeal airways help maintain airway patency, especially during prolonged ventilation.
Mastering the Mask Seal
Creating an effective seal between the mask and face prevents air leakage and ensures adequate ventilation. The EC-clamp technique proves most effective: use your thumb and index finger to form a “C” around the mask while your remaining three fingers form an “E” that lifts the jaw upward toward the mask.
Two-person bag valve mask ventilation often works better than the single-rescuer technique. One provider maintains the mask seal using both hands while the second squeezes the bag. Research confirms this approach provides more effective ventilation when significant airway obstruction or poor lung compliance exists.
Delivering Appropriate Tidal Volumes
The guiding principle remains delivering the smallest effective tidal volume that produces a visible chest rise. For pediatric patients, the target is 4-6 milliliters per kilogram of body weight. Visual chest rise serves as the most reliable indicator of proper ventilation.
Over-inflation causes serious complications, including barotrauma, pneumothorax, and gastric insufflation. The latter increases aspiration risk and impairs ventilation by elevating the diaphragm. Healthcare providers commonly deliver excessive ventilation during CPR, particularly when advanced airways are in place. This hyperventilation proves harmful as it increases intrathoracic pressure and decreases venous return to the heart.
Current Guidelines for Pediatric Bag Valve Mask Ventilation
Ventilation Rates During Resuscitation
The American Heart Association recommends specific ventilation rates based on the clinical scenario. After advanced airway placement or during isolated respiratory arrest, deliver 20-30 breaths per minute (one breath every 2-3 seconds). During cardiac arrest with bag valve mask ventilation, pair ventilations with chest compressions.
For single-rescuer situations, use a compression-to-ventilation ratio of 30:2 for all patients. When two or more rescuers are available, the ratio changes to 15:2 for pre-pubertal patients while remaining 30:2 for post-pubertal patients. Deliver ventilations with minimal interruptions in chest compressions.
Monitoring Ventilation Quality
End-tidal carbon dioxide monitoring provides valuable feedback on ventilation efficacy and cardiac output during CPR. A sudden rise in ETCO2 may indicate a return of spontaneous circulation. However, the 2025 guidelines explicitly state that ETCO2 should not be used when deciding whether to discontinue resuscitative efforts.
When arterial lines are in place, utilize diastolic pressure measurements to guide resuscitation. Target diastolic pressure greater than 25 mm Hg in infants under one year and greater than 30 mm Hg in older children. CPR feedback devices providing audio and audiovisual cues may improve compression and ventilation quality within comprehensive training systems.
Common Pitfalls and How to Avoid Them
Preventing Barotrauma
Barotrauma represents one of the most serious complications of bag valve mask ventilation. Excessive airway pressures cause alveolar damage, potentially leading to pneumothorax, pneumomediastinum, or subcutaneous emphysema. Healthcare providers should maintain plateau pressures below 30 cm H2O when possible.
Watch for signs of over-ventilation, including decreased breath sounds on one side, sudden patient deterioration, or subcutaneous emphysema. If chest rise appears adequate but resistance increases, check for proper mask seal and airway positioning before increasing ventilation pressure.
Managing Gastric Insufflation
Gastric insufflation occurs when air enters the stomach rather than the lungs. This complication elevates the diaphragm, impairs ventilation, and increases aspiration risk. Prevent gastric insufflation by maintaining appropriate inspiratory pressures and delivering breaths over 1 second.
If significant gastric distension occurs, consider inserting a nasogastric or orogastric tube to decompress the stomach. Never apply excessive force when squeezing the bag, as this increases both barotrauma and gastric insufflation risks.
Recognizing Equipment Limitations
Many pediatric BVMs include pop-off valves designed to prevent excessive pressures. While these valves provide important safety protection, they may prevent adequate ventilation in patients with poor lung compliance or significant airway obstruction. Some devices allow bypassing the pop-off valve, but only trained clinicians should disable this safety feature with continuous monitoring.
If the chest rise remains inadequate despite a good seal and proper positioning, troubleshoot systematically. Adjust mask fit, reposition the head, insert an airway adjunct, and suction secretions. Only bypass pressure-relief valves when necessary and with senior provider support.
Training and Skill Maintenance for Pediatric Bag Valve Mask Proficiency
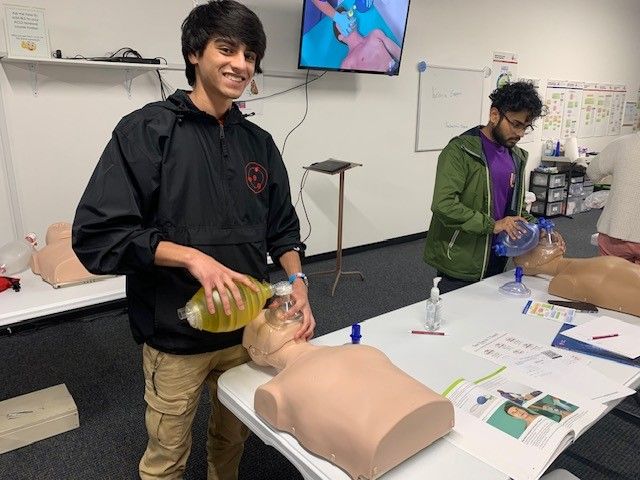
Healthcare providers must recognize that bag-valve-mask ventilation appears simple in theory but is difficult in practice. Quality depends heavily on provider skill and regular practice. Studies demonstrate that skills deteriorate quickly without consistent reinforcement.
High-frequency, feedback-based practice provides the best safeguard against preventable errors. Real-time feedback devices that measure tidal volume, rate, and pressure help providers develop proper technique. Scenario-based drills addressing mask leaks, stiff lungs, and obstructed airways build confidence and competence.
The American Heart Association emphasizes hands-on training under qualified instructors. Proper certification programs ensure providers develop both knowledge and practical skills needed to respond effectively during critical situations. Regular recertification maintains competency and introduces updated guidelines.
Take Action: Strengthen Your Pediatric Resuscitation Skills
Mastering pediatric bag valve mask ventilation requires commitment to ongoing education and practice. Your ability to perform this critical skill confidently can mean the difference between life and death for a child in respiratory distress.
CPR Nashville, an American Heart Association training site, offers comprehensive PALS classes in Nashville that cover pediatric bag valve mask ventilation techniques alongside other essential pediatric resuscitation skills. All classes are stress-free and hands-on, ensuring you develop real-world competence.
Whether you need initial certification or renewal in BLS for Healthcare Providers, ACLS, PALS, or CPR and First Aid, CPR Nashville provides the expert instruction you need. Don’t wait until an emergency occurs to wish you had better training.
Enroll in PALS classes in Nashville today or secure your CPR certification in Nashville to gain the confidence and skills required for effective pediatric emergency response. Visit CPR Nashville now to register for upcoming courses and take the next step in protecting the children in your care.