In the field of emergency medicine, few techniques hold as much life-saving potential as cardiopulmonary resuscitation (CPR). This critical procedure has been a cornerstone of resuscitation efforts for decades, and its evolution has been driven by continuous research, innovative approaches, and a commitment to improving patient outcomes. As medical professionals, it’s imperative to stay informed about the latest developments and updates in CPR techniques to ensure we deliver the most effective care possible.
Over the years, CPR guidelines have undergone numerous revisions, reflecting our growing understanding of the science behind resuscitation and the ever-evolving best practices. These updates are the result of extensive research, clinical trials, and the collective expertise of medical professionals worldwide, all working towards a common goal: increasing the chances of survival for those in cardiac arrest.
One of the most significant recent changes in CPR techniques concerns the compression technique itself. The American Heart Association’s latest guidelines emphasize the importance of delivering high-quality chest compressions with the correct rate and depth. Specifically, compressions should be administered at a rate of 100-120 per minute, with a depth of at least 2 inches for adults and about 1.5 inches for infants.
Proper compression technique is essential for ensuring adequate blood flow and oxygenation during cardiac arrest. The updated guidelines also stress the importance of minimizing interruptions in chest compressions, as even brief pauses can significantly reduce the effectiveness of CPR. To achieve this, new techniques have been introduced, such as the “pit crew” approach, which emphasizes efficient teamwork and coordination during resuscitation efforts.
In addition to changes in compression technique, the breathing component of CPR has also undergone revisions. For certain situations, such as when only a single rescuer is available, the guidelines now recommend prioritizing continuous chest compressions over rescue breaths. This approach, known as “compression-only CPR,” is effective in improving survival rates, particularly in the critical first few minutes of cardiac arrest.
However, it’s important to note that for specific populations, such as infants and children, rescue breaths remain a crucial part of the CPR sequence. The guidelines provide tailored approaches for these groups, recognizing the unique physiological needs and considerations involved in pediatric resuscitation.
Historical Evolution of CPR
Cardiopulmonary Resuscitation (CPR) traces its roots back through centuries of medical innovation and human ingenuity. While the concept of artificial respiration and chest compression dates back to ancient civilizations, the modern form of CPR as we know it today began to take shape in the mid-20th century.
Origins of CPR
- Ancient Techniques: Throughout history, various civilizations employed techniques to revive unconscious individuals, including mouth-to-mouth resuscitation and chest compressions. Records from ancient Egypt, Greece, and Rome depict early attempts at resuscitation.
- The Renaissance: During the Renaissance period, scholars such as Andreas Vesalius conducted anatomical studies that laid the groundwork for understanding the human body’s physiology, including the circulation of blood and the function of the heart and lungs.
Milestones in CPR Development
- The 18th Century: The concept of artificial respiration gained traction in the 18th century, with techniques such as the Silvester Method, which involved positioning the patient and manipulating their arms and chest to facilitate breathing.
- The 20th Century: CPR as we know it began to take shape in the 20th century with the introduction of closed-chest cardiac massage by Dr. James Elam and Dr. Peter Safar in the 1950s. This technique involved external chest compressions to manually circulate blood in the event of cardiac arrest.
- In the 1960s: Dr. Kouwenhoven, Dr. Jude, and Dr. Knickerbocker developed the “cardiac massage” technique, which involved the combination of chest compressions and mouth-to-mouth resuscitation. This laid the foundation for modern CPR protocols.
- The 1970s: The American Heart Association (AHA) introduced the first standardized CPR guidelines in 1973, emphasizing the importance of chest compressions and rescue breathing. This marked a significant milestone in the widespread adoption of CPR training programs.
Impact of Research and Technological Advancements
- Research Initiatives: Ongoing research in the fields of cardiology, emergency medicine, and resuscitation science continues to refine and improve CPR techniques. Studies have led to a deeper understanding of optimal compression rates, depth, and hand placement.
- Technological Innovations: The advent of automated external defibrillators (AEDs) has revolutionized CPR interventions by providing accessible, user-friendly devices that can deliver electrical shocks to restore normal heart rhythms in cardiac arrest patients.
Current Standard CPR Techniques
In recent decades, CPR techniques have evolved to prioritize simplicity, efficiency, and effectiveness. The current standard CPR protocols, endorsed by organizations such as the American Heart Association (AHA) and the European Resuscitation Council (ERC), emphasize a combination of chest compressions and rescue breaths tailored to the needs of the victim.
Basic CPR Procedure
- Recognition of Cardiac Arrest: The first step in administering CPR is to recognize the signs of cardiac arrest, including unresponsiveness, absence of breathing, and lack of pulse.
- Activation of Emergency Response: Upon recognizing cardiac arrest, it is essential to activate the emergency medical services (EMS) system by calling for help or instructing someone else to do so.
- Chest Compressions: The cornerstone of CPR is high-quality chest compressions. Rescuers should place the heel of one hand on the center of the victim’s chest (lower half of the sternum) and interlock the fingers of the other hand. Compressions should be delivered at a rate of 100 to 120 compressions per minute, allowing the chest to recoil fully between compressions.
- Rescue Breaths (Ventilations): In traditional CPR, rescue breaths are administered in conjunction with chest compressions. Rescuers should deliver two breaths into the victim’s mouth, ensuring a visible chest rise with each breath.
Differences Between CPR for Healthcare Providers and Laypersons
- Healthcare Provider CPR (BLS): CPR training for healthcare providers includes additional skills such as advanced airway management, the use of bag-mask ventilation, and the administration of medications. Healthcare providers are trained to perform CPR as part of a team and may use specialized equipment such as defibrillators and advanced airway devices.
- Layperson CPR: Layperson CPR focuses on teaching bystanders and non-medical personnel the essential skills needed to respond to cardiac emergencies. Layperson CPR courses typically emphasize hands-on CPR, which involves continuous chest compressions without rescue breaths for adults in cardiac arrest.
Importance of AED (Automated External Defibrillator) Use
- Early Defibrillation: AEDs play a crucial role in the chain of survival for cardiac arrest victims. These portable devices are designed to analyze the heart rhythm and deliver a shock if necessary to restore normal cardiac function.
- Accessibility and Training: AEDs are becoming increasingly accessible in public spaces, including schools, airports, and workplaces. Training in AED use is integral to CPR courses, empowering bystanders to take immediate action in cardiac emergencies.
Recent Innovations in CPR
While the fundamental principles of CPR remain unchanged, recent innovations in resuscitation science have focused on optimizing techniques to maximize outcomes for cardiac arrest patients. These innovations aim to simplify CPR delivery, increase bystander intervention, and improve the quality of compressions and ventilations.
Hands-Only CPR
- Simplified Technique: Hands-only CPR, also known as compression-only CPR, involves continuous chest compressions without rescue breaths. This technique simplifies CPR delivery, making it easier for bystanders to initiate CPR and maintain compressions until help arrives.
- Effectiveness: Research has shown that hands-on CPR can be as effective as traditional CPR, particularly in cases of adult cardiac arrest due to sudden cardiac events. The American Heart Association recommends hands-on CPR for untrained bystanders or individuals unwilling to perform rescue breaths.
Continuous Chest Compression CPR
- Minimizing Interruptions: Continuous chest compression CPR focuses on minimizing interruptions to chest compressions during CPR delivery. This technique prioritizes chest compressions over rescue breaths, with brief interruptions only for rhythm checks and defibrillator use.
- Improved Perfusion: By maintaining uninterrupted blood flow to vital organs, continuous chest compression CPR may improve the chances of restoring spontaneous circulation and achieving favorable outcomes in cardiac arrest patients.
Use of Technology in CPR Training
-
Virtual Reality (VR) Training: Virtual reality platforms offer immersive CPR training experiences that simulate real-life scenarios. Learners can practice CPR techniques in virtual environments, receiving instant feedback on their performance and enhancing skill retention. VR training enhances engagement and confidence among participants, ultimately improving the quality of CPR delivery in clinical settings.
- Mobile Applications: CPR training applications provide convenient access to educational resources and step-by-step guides for performing CPR. These apps often include interactive tutorials, practice sessions, and certification options, empowering individuals to learn CPR skills at their own pace and convenience. Mobile applications serve as valuable tools for ongoing training and skill maintenance, particularly for laypersons and healthcare professionals.
Importance of Early Recognition and Response
- Community CPR Programs: Community-based CPR initiatives aim to increase public awareness and bystander intervention in cardiac emergencies. These programs offer CPR training to individuals in schools, workplaces, and community centers, equipping communities with the knowledge and skills needed to respond effectively to cardiac arrest incidents. By empowering bystanders to recognize cardiac arrest and initiate CPR promptly, community CPR programs contribute to improved survival rates and outcomes.
- Integration with Telecommunication Systems: Integration of CPR instructions with emergency dispatch systems enables dispatchers to provide real-time guidance to callers performing CPR. Dispatch-assisted CPR instructions help bystanders initiate CPR promptly and perform high-quality chest compressions until emergency medical services (EMS) arrive on the scene. This integration enhances the coordination of care and optimizes patient outcomes in time-sensitive cardiac emergencies.
Specialized CPR Techniques
While basic CPR techniques are essential for responding to most cardiac emergencies, specialized CPR techniques are tailored to specific populations or scenarios, such as infants, children, and advanced cardiac life support situations. These specialized techniques ensure that responders can adapt their approach to provide the most effective care for patients in diverse circumstances.
CPR Techniques for Infants and Children (Pediatric CPR)
- Differences in Anatomy: Infants and children have anatomical differences that necessitate modifications to CPR techniques. For example, rescuers should use two fingers for chest compressions in infants and the heel of one hand in young children to achieve appropriate compression depth.
- Pediatric Chain of Survival: Pediatric CPR emphasizes the importance of early recognition, activation of emergency response, high-quality chest compressions, and rapid defibrillation when necessary. Pediatric Advanced Life Support (PALS) protocols provide guidelines for managing pediatric cardiac emergencies.
Advanced CPR Techniques
- Advanced Cardiovascular Life Support (ACLS): ACLS is a set of advanced resuscitation protocols designed for healthcare providers managing cardiac arrest and other life-threatening emergencies. ACLS algorithms guide the management of cardiac rhythms, medication administration, and advanced airway management.
- Pediatric Advanced Life Support (PALS): PALS protocols address the unique needs of pediatric patients in cardiac arrest or other critical conditions. PALS training focuses on rapid assessment, effective team dynamics, and interventions specific to pediatric resuscitation.
CPR in Special Circumstances
- Drowning: CPR techniques for drowning victims may involve clearing the airway of water and providing rescue breaths along with chest compressions. Prompt initiation of CPR is crucial to improve outcomes in drowning emergencies.
- Choking: Choking victims may require abdominal thrusts (Heimlich maneuver) or back blows to dislodge obstructing objects. If choking leads to cardiac arrest, CPR should be initiated immediately.
Challenges and Considerations
Despite the advancements in CPR techniques and training programs, several challenges and considerations persist in the realm of cardiopulmonary resuscitation. Addressing these challenges is crucial for optimizing the delivery of CPR and improving outcomes for cardiac arrest patients.
Barriers to Effective CPR Administration
- Fear and Uncertainty: Fear of causing harm or uncertainty about performing CPR correctly can deter bystanders from initiating resuscitation efforts. Overcoming these psychological barriers through education, training, and public awareness campaigns is essential to promote bystander intervention in cardiac emergencies.
- Compression Quality: Maintaining high-quality chest compressions, including adequate depth, rate, and recoil, remains a challenge for responders, particularly in high-stress environments. Continuous feedback devices and real-time performance monitoring can help improve compression quality and consistency during CPR delivery.
Importance of Regular Training and Certification Renewal
- Skill Degradation: CPR skills may degrade over time without regular practice and reinforcement. Healthcare providers and laypersons alike must undergo recurrent training and certification renewal to stay proficient in CPR techniques and updates in resuscitation guidelines.
- Integration into Professional Practice: Healthcare organizations must prioritize CPR training and integration of resuscitation protocols into clinical practice. Providing ongoing education and support for healthcare professionals ensures that CPR is performed effectively as part of routine patient care.
Addressing Misconceptions and Fears About CPR
- Education and Awareness: Misconceptions about CPR, such as the perceived complexity or invasiveness of the procedure, can hinder bystander willingness to intervene in cardiac emergencies. Comprehensive CPR education and public awareness campaigns are essential for dispelling myths and fostering a culture of proactive response to cardiac arrest.
- Legal Protection and Good Samaritan Laws: Clarifying the legal protections afforded to bystanders who perform CPR is critical for mitigating fears of liability. Good Samaritan laws, which shield individuals from legal liability when providing emergency assistance in good faith, play a crucial role in encouraging bystander intervention and removing legal barriers to CPR administration.
Future Directions in CPR
As technology advances and our understanding of resuscitation science deepens, the future of cardiopulmonary resuscitation (CPR) holds promise for further innovation and improvement in life-saving techniques. From advancements in device technology to novel approaches in training and education, several avenues are poised to shape the future of CPR and enhance outcomes for cardiac arrest patients.
Emerging Technologies in CPR Devices
- Next-Generation Defibrillators: Continued innovation in defibrillator technology may lead to the development of more compact, user-friendly devices with enhanced diagnostic capabilities. Integration of artificial intelligence algorithms and machine learning may enable defibrillators to provide real-time feedback and personalized treatment recommendations during cardiac arrest resuscitation.
- Sensor Technology: Wearable sensors and monitoring devices have the potential to revolutionize CPR delivery by providing continuous physiological feedback to rescuers. These sensors can monitor chest compression quality, patient vital signs, and response to resuscitation efforts, allowing for real-time optimization of CPR interventions.
Integration of CPR into Public Health Initiatives
- Community-Based CPR Programs: The expansion of community-based CPR training programs and public access to defibrillators (PADs) can significantly increase bystander intervention rates and survival outcomes in cardiac emergencies. Collaborative efforts between healthcare providers, government agencies, and community organizations are essential for implementing and sustaining these initiatives.
- Mobile Health (mHealth) Solutions: Mobile health applications and platforms offer opportunities to disseminate CPR education, training, and real-time assistance to a wider audience. Leveraging smartphones and digital platforms, mHealth solutions can empower individuals to learn CPR skills, receive CPR alerts, and connect with emergency response systems in cardiac emergencies.
Potential Advancements in CPR Education and Training Methodologies
- Simulation-Based Training: Advancements in simulation technology, including virtual reality (VR) and augmented reality (AR), may revolutionize CPR training by providing immersive, hands-on learning experiences. Simulation-based training allows learners to practice CPR skills in realistic scenarios, receive instant feedback, and refine their performance in a safe and controlled environment.
- Remote Training and Telemedicine: Remote training platforms and telemedicine services offer opportunities for remote CPR education and certification, particularly in underserved or remote communities. Virtual training sessions, interactive webinars, and teleconsultations with CPR instructors enable individuals to access high-quality training and support from anywhere with internet connectivity.
Conclusion
The evolution of cardiopulmonary resuscitation (CPR) reflects humanity’s relentless pursuit of innovation and excellence in the realm of life-saving techniques. From its humble origins to the forefront of modern resuscitation science, CPR has undergone remarkable transformations, driven by advancements in technology, research, and education.
In conclusion, the journey of CPR evolution underscores the importance of readiness and proficiency in life-saving techniques. Whether you’re a healthcare professional or a concerned citizen, obtaining CPR certification is a vital step in equipping yourself to respond effectively in cardiac emergencies.
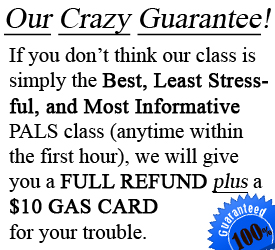
At CPR Classes Tampa, an accredited American Heart Association training site, you’ll find the resources and expertise you need to become CPR-certified. Offering a range of courses, including BLS for Healthcare Providers, ACLS, PALS, and CPR and First Aid, CPR Classes Tampa ensures that you receive top-notch training in a stress-free, hands-on environment. With its dedication to excellence, CPR Classes Tampa stands as the premier destination for CPR certification in Tampa.
Take action today and enroll in CPR certification courses at CPR Classes Tampa. By becoming CPR certified, you’re not just acquiring a skill; you’re joining a community of trained responders committed to saving lives in our community. Don’t delay—invest in your CPR certification with CPR Classes Tampa and be prepared to make a difference when it matters most.