Each year, approximately 350,000 Americans experience out-of-hospital cardiac arrest (OHCA), yet fewer than 10% survive to hospital discharge. The difference between life and death often hinges on one critical factor: early recognition. When bystanders quickly identify cardiac arrest and initiate the BLS algorithm, survival rates increase dramatically. Recent data from the 2024 Cardiac Arrest Registry to Enhance Survival (CARES) reveals that patients whose arrests were witnessed by bystanders were more than three times more likely to survive than those whose arrests went unwitnessed (16.0% versus 4.5%).
Early recognition serves as the first vital link in the chain of survival. Without it, even the most advanced medical interventions arrive too late. The BLS algorithm begins with recognizing unresponsiveness and abnormal breathing, two key indicators that immediate action is needed. Healthcare providers and trained rescuers must distinguish between cardiac arrest, respiratory arrest, and other medical emergencies within seconds.
The 2025 American Heart Association Guidelines emphasize that early recognition, combined with high-quality CPR, represents the cornerstone of neurologically intact survival. Studies show that for every minute without CPR intervention, survival chances decrease by 7-10%. This statistic underscores why immediate recognition cannot be delayed or second-guessed.
Understanding the BLS Algorithm and Early Assessment
The BLS algorithm provides a systematic approach to cardiac emergency response. It starts with a scene safety assessment, followed by checking for responsiveness, activating the emergency response system, and checking for breathing and pulse simultaneously within 10 seconds. This rapid assessment determines whether the patient is in cardiac arrest or experiencing another medical emergency.
According to the latest guidelines, the BLS algorithm emphasizes CAB (Chest compressions, Airway, Breathing) rather than ABC. This change reflects research showing that chest compressions must begin immediately to maintain blood flow to vital organs. The algorithm guides responders through: checking responsiveness, calling for help, assessing pulse and breathing, starting chest compressions, opening the airway, delivering rescue breaths, and using an automated external defibrillator (AED) when available.
Healthcare providers trained in the BLS algorithm know that agonal gasps, which occur in up to 40% of cardiac arrests, should not be mistaken for normal breathing. These irregular, gasping breaths indicate cardiac arrest and require immediate CPR. Research from the Danish Cardiac Arrest Registry shows that when OHCA is recognized during emergency calls, bystander CPR increases significantly (odds ratio of 7.84), leading to improved return of spontaneous circulation and 30-day survival.
The BLS algorithm also addresses specific scenarios like respiratory arrest, where patients have a pulse but inadequate breathing. Early recognition of this condition prevents progression to cardiac arrest. Immediate interventions include opening the airway, providing ventilation at the appropriate rate, and continuously monitoring for deterioration.
The Time-Critical Nature of Recognition in BLS
Time represents the enemy in cardiac arrest situations. Recent research presented at the American Heart Association’s 2024 Resuscitation Science Symposium demonstrates that CPR initiated within two minutes of cardiac arrest increases survival chances by 81% compared to no bystander CPR. Even more striking, patients receiving CPR within the first two minutes showed a 95% higher chance of surviving without significant brain damage.
The benefits of early BLS intervention decrease as time passes. Data shows that bystander CPR remains effective up to 10 minutes after cardiac arrest, but the advantage diminishes beyond this threshold. People who received CPR more than 10 minutes after cardiac arrest showed no higher survival rates than those who received no CPR at all. This evidence reinforces that rapid recognition and immediate action are paramount.
The Swedish Cardiac Arrest Registry, which tracks more than 90% of all out-of-hospital cardiac arrests in Sweden, provides compelling evidence about timing. When CPR was performed before emergency medical services (EMS) arrival, the 30-day survival rate reached 10.5%, compared to only 4.0% when CPR was not initiated until EMS arrived. This finding demonstrates the life-saving impact of early bystander recognition and intervention.
In-hospital cardiac arrest data also supports the importance of early recognition. The American Heart Association’s Get With The Guidelines-Resuscitation data shows that survival to hospital discharge for adult in-hospital cardiac arrest patients reached 23.6% in 2023, with 79.2% of survivors achieving favorable neurologic outcomes. This success stems partly from healthcare professionals’ ability to recognize early signs of patient deterioration and intervene before cardiac arrest occurs.
How Bystander Recognition Improves BLS Algorithm Outcomes
Bystander intervention plays a pivotal role in cardiac arrest survival. The 2024 CARES data indicate that bystander CPR was initiated in 41.7% of reported OHCA cases. When bystanders provided CPR, survival to hospital discharge increased to 13.0%, compared to only 7.6% among patients who did not receive bystander assistance.
Training civilians to recognize cardiac arrest symptoms has become a public health priority. Several states have achieved remarkable bystander CPR rates: Alaska leads at 79.7%, followed by Nevada (57.5%), Oregon (54.6%), and Washington (53.6%). These high intervention rates correlate with improved community survival outcomes, demonstrating that widespread BLS training creates life-saving communities.
Recognition training must address common barriers. Approximately 70% of Americans express hesitation to perform CPR due to lack of training or lapsed knowledge. Additionally, research reveals disparities in bystander intervention: Black and Hispanic individuals are less likely to receive bystander CPR both at home and in public settings compared to white individuals. These disparities contribute to lower survival rates in marginalized communities.
The role of telecommunicators in facilitating early recognition cannot be overstated. When emergency dispatchers recognize cardiac arrest during calls, they can provide telephone CPR instructions, dramatically increasing bystander intervention rates. Studies show that addressing breathing patterns and ensuring callers are positioned by the patient’s side significantly improve cardiac arrest recognition during emergency calls.
Evidence-Based Strategies for Improving Early Recognition
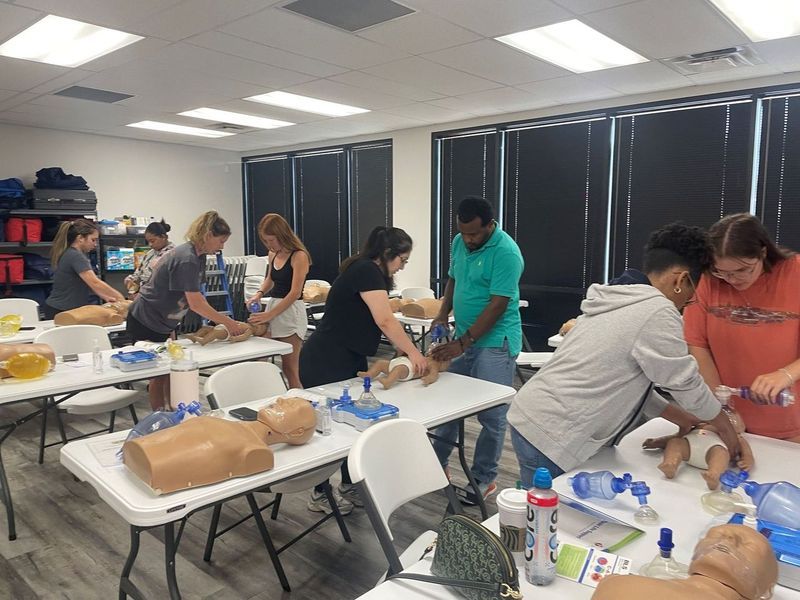
Healthcare organizations and communities can implement several evidence-based strategies to enhance early recognition capabilities. First, comprehensive BLS training programs should emphasize recognition skills, not just technical CPR skills. Participants need practice distinguishing cardiac arrest from other emergencies, identifying agonal breathing, and overcoming hesitation to act.
Mobile phone technology offers innovative solutions for improving recognition and response times. Alert systems that recruit trained laypeople in the vicinity of cardiac arrests show significant advantages in practicing effective CPR. These systems leverage GPS technology to dispatch citizen responders who can begin CPR while professional help is en route.
Public access defibrillation programs expand recognition and intervention beyond healthcare settings. With more than 15% of OHCAs occurring in public locations, strategically placed AEDs combined with community training create a safety net. States with higher bystander AED use, including Nebraska (21.4%) and Nevada (19%), demonstrate the impact of accessible defibrillation technology.
Healthcare facilities can improve in-hospital cardiac arrest outcomes by implementing early warning systems that identify patient deterioration. The notable increase in pediatric survival from 18.9% to 45.2% between 2000 and 2023 is attributed to multiple factors, including early recognition of deterioration and provision of high-quality CPR.
The 2025 American Heart Association Guidelines introduce several updates to the BLS algorithm, including recommendations for naloxone use by lay rescuers during respiratory and cardiac arrest. These updates reflect an evolving understanding of cardiac arrest causes and appropriate recognition criteria. Healthcare providers must stay current with these changes through regular recertification and continuing education.
The Broader Impact of Recognition on the Chain of Survival
Early recognition activates the entire chain of survival, which includes: immediate recognition and activation of emergency response, early CPR, rapid defibrillation, effective advanced life support, post-cardiac arrest care, and recovery support. Each link depends on the previous one, making recognition the critical starting point.
The American Heart Association’s 2030 Emergency Cardiovascular Care Goals aim to eliminate disparities in bystander CPR, AED use, and survival across race, ethnicity, income, sex, gender, and geographic location. Achieving these goals requires focused efforts on improving recognition training in underserved communities and addressing barriers that prevent timely intervention.
Post-resuscitation outcomes increasingly depend on the quality of initial recognition and BLS provision. Patients who receive early, high-quality CPR have better neurological outcomes, higher quality of life, and improved chances of returning to work and participating in society. The economic and social benefits of early recognition extend beyond immediate survival to encompass long-term recovery and rehabilitation.
Communities with integrated systems of care, combining public education, telecommunicator CPR programs, and rapid EMS response, achieve the best outcomes. These systems recognize that cardiac arrest is not just a medical emergency but a community health challenge requiring widespread participation and preparedness.
Take Action: Master Early Recognition Through Professional BLS Training
Understanding the importance of early recognition is just the first step. Translating this knowledge into action requires hands-on training, regular practice, and confidence-building experience. Every second counts during cardiac arrest, and your ability to quickly recognize the signs and implement the BLS algorithm can mean the difference between life and death.
Don’t wait for an emergency to wish you had proper training. CPR Classes Tampa, an American Heart Association training site, offers comprehensive BLS for Healthcare Providers, ACLS, PALS, and CPR and First Aid courses designed to build your recognition and intervention skills. All classes are stress-free, hands-on, and taught by experienced instructors who ensure you gain the confidence to act when it matters most.
Whether you need initial CPR certification in Tampa or are due for renewal, our courses provide the latest evidence-based training aligned with current guidelines. Healthcare professionals seeking BLS classes in Tampa will benefit from advanced recognition training that goes beyond basic life support to address complex cardiac emergencies.
The statistics are clear: early recognition saves lives, and proper training makes early recognition possible. Join the thousands of healthcare providers and community members who have empowered themselves with life-saving skills. Contact CPR Classes Tampa today to schedule your certification course and become part of the solution to improving cardiac arrest survival in our community.
Frequently Asked Questions About Early Recognition in BLS
Q: How quickly must I recognize cardiac arrest to make a difference in survival outcomes?
Research shows you must recognize cardiac arrest and begin CPR within the first 2-10 minutes for optimal outcomes. CPR started within two minutes increases survival chances by 81% and dramatically improves neurological outcomes. Even CPR initiated within 10 minutes provides survival benefits, though effectiveness decreases as time passes. For every minute without CPR, survival chances drop by 7-10%, which means immediate recognition is critical. The BLS algorithm emphasizes checking for responsiveness and abnormal breathing within seconds, enabling you to start chest compressions without delay.
Q: What are the key signs I should recognize that indicate someone needs the BLS algorithm?
The primary signs requiring immediate BLS algorithm activation include unresponsiveness, absence of normal breathing (or only agonal gasps), and no detectable pulse. When assessing a potential cardiac arrest victim, check for responsiveness by tapping and shouting. Simultaneously check for breathing and pulse within 10 seconds. Remember that agonal gasps occur in up to 40% of cardiac arrests and should not be confused with normal breathing. If the person is unresponsive and not breathing normally, immediately activate emergency services and begin chest compressions. Do not waste time trying to confirm a pulse if you’re uncertain—it’s safer to start CPR.
Q: How does early recognition during the BLS algorithm affect long-term neurological outcomes?
Early recognition profoundly impacts brain function preservation. When cardiac arrest occurs, the brain begins suffering irreversible damage within 4-6 minutes without oxygenated blood flow. Patients who receive bystander CPR within two minutes have a 95% higher chance of surviving without significant brain damage compared to those who receive no CPR. The 2023 data from Get With The Guidelines-Resuscitation shows that 79.2% of adult in-hospital cardiac arrest survivors achieved favorable neurologic outcomes, partly due to healthcare professionals’ early recognition of deterioration. High-quality CPR initiated immediately after recognition maintains some blood flow to the brain, preserving neurological function until advanced care arrives.
Q: What role does BLS algorithm training play in improving my recognition skills during real emergencies?
Formal BLS algorithm training dramatically improves recognition speed and accuracy by providing hands-on practice with realistic scenarios. Studies show that trained responders are significantly more likely to recognize cardiac arrest quickly and act appropriately. Training addresses common recognition challenges, including distinguishing agonal breathing from normal respirations, overcoming hesitation, and correctly assessing responsiveness. Communities with high rates of BLS training demonstrate better survival outcomes—states like Alaska (79.7% bystander CPR rate) and Nevada (57.5%) show that widespread training translates to more lives saved. Regular recertification (every 1-2 years) keeps recognition skills sharp and ensures you’re familiar with updated guidelines. Professional courses like those offered at CPR Classes Tampa provide the repetitive practice needed to build muscle memory and confidence for real-world application.




