Understanding the Critical Window After Return of Spontaneous Circulation
When a patient achieves return of spontaneous circulation (ROSC) following cardiac arrest, healthcare providers face a critical challenge. The H’s and T’s framework provides a systematic approach to identifying and treating reversible causes that may have triggered the initial arrest or could cause re-arrest.
Successfully diagnosing causes using the H’s and T’s methodology can mean the difference between sustained recovery and repeated cardiac events. This evidence-based approach ensures that no potentially treatable condition goes unrecognized during the vulnerable post-ROSC period.
The H’s: Hypoxic and Metabolic Causes of Cardiac Arrest
Hypoxia: The Silent Threat
Hypoxia remains one of the most common reversible causes encountered in cardiac arrest scenarios. Post-ROSC, inadequate oxygenation can quickly precipitate another arrest. Healthcare providers must immediately assess airway patency, breathing adequacy, and oxygen saturation levels.
Signs of ongoing hypoxia include cyanosis, altered mental status, and persistent tachycardia. Treatment involves securing the airway, providing supplemental oxygen, and addressing underlying respiratory pathology. The H’s and T’s framework emphasizes rapid identification and correction of hypoxic states.
Hypovolemia: Recognizing Volume Depletion
Severe volume depletion can lead to cardiac arrest through inadequate preload and subsequent cardiovascular collapse. In the post-ROSC phase, diagnosing causes related to hypovolemia requires careful assessment of fluid status and hemodynamic parameters.
Clinical indicators include flat neck veins, dry mucous membranes, and poor skin turgor. Additionally, tachycardia with narrow pulse pressure may suggest volume depletion. Treatment involves rapid fluid resuscitation with crystalloids or blood products as appropriate.
Hyperkalemia and Hypokalemia: Electrolyte Emergencies
Potassium imbalances represent critical diagnostic causes within the H’s and T’s framework. Hyperkalemia can cause wide-complex rhythms leading to cardiac arrest, while severe hypokalemia predisposes patients to dangerous arrhythmias.
Post-ROSC electrocardiograms may reveal peaked T-waves in hyperkalemia or flattened T-waves with prominent U-waves in hypokalemia. Immediate laboratory studies and appropriate electrolyte correction are essential for preventing re-arrest.
Hypothermia: Temperature-Related Cardiac Events
Severe hypothermia can precipitate cardiac arrest through various mechanisms, including increased cardiac irritability and metabolic depression. When diagnosing causes post-ROSC, core temperature measurement is crucial, especially in environmental exposure cases.
Treatment involves gradual rewarming techniques while monitoring for potential complications such as the afterdrop phenomenon. The H’s and T’s approach emphasizes careful temperature management in hypothermic cardiac arrest patients.
The T’s: Mechanical and Toxic Causes
Tension Pneumothorax: Immediate Life Threat
Tension pneumothorax represents a rapidly fatal condition that can cause cardiac arrest through impaired venous return and reduced cardiac output. The H’s and T’s framework prioritizes immediate recognition and treatment of this mechanical cause.
Clinical signs include unilateral absence of breath sounds, tracheal deviation, and jugular venous distension. Emergency needle decompression followed by chest tube placement can be life-saving interventions in the post-ROSC period.
Tamponade: Pericardial Emergency
Cardiac tamponade involves fluid accumulation in the pericardial space, leading to impaired cardiac filling and potential arrest. Diagnosing causes related to tamponade requires high clinical suspicion and appropriate diagnostic tools.
Beck’s triad (elevated venous pressure, hypotension, and muffled heart sounds) may be present, but is not always complete. Echocardiography provides a definitive diagnosis, while pericardiocentesis offers therapeutic intervention for this treatable cause.
Toxins: Poisoning and Overdose
Various toxins can precipitate cardiac arrest through different mechanisms, including sodium channel blockade, calcium channel antagonism, and direct myocardial depression. The H’s and T’s approach emphasizes obtaining detailed exposure history when diagnosing causes.
Common culprits include tricyclic antidepressants, calcium channel blockers, and beta-blockers. Treatment involves specific antidotes when available, supportive care, and potentially extracorporeal membrane oxygenation in severe cases.
Thrombosis: Coronary and Pulmonary
Both coronary thrombosis (heart attack) and pulmonary thromboembolism can cause cardiac arrest through different pathophysiologic mechanisms. The H’s and T’s framework guides systematic evaluation for these vascular emergencies.
Coronary thrombosis requires immediate reperfusion therapy through percutaneous coronary intervention or thrombolytic therapy. Massive pulmonary embolism may necessitate emergent embolectomy or thrombolytic treatment for optimal outcomes.
Systematic Approach to Post-ROSC Evaluation
Implementing the H’s and T’s methodology requires a structured approach to patient assessment. Healthcare providers should systematically evaluate each potential cause while simultaneously providing supportive care and monitoring for signs of deterioration.
Laboratory studies should include arterial blood gas analysis, complete metabolic panel, cardiac enzymes, and coagulation studies. Imaging studies such as chest X-ray, echocardiogram, and CT scanning may provide crucial diagnostic information for identifying reversible causes.
The effectiveness of diagnosing causes using this framework depends on rapid implementation and team coordination. Every member of the resuscitation team should understand the H’s and T’s approach and contribute to the systematic evaluation process.
Long-term Outcomes and Prevention Strategies
Successful identification and treatment of reversible causes using the H’s and T’s framework significantly improve patient outcomes. Studies demonstrate that addressing these underlying conditions reduces the likelihood of recurrent cardiac arrest and improves overall survival rates.
Prevention strategies focus on early recognition of high-risk conditions, appropriate monitoring, and prompt intervention when warning signs develop. Healthcare systems should implement protocols that facilitate rapid H’s and T’s assessment in all cardiac arrest cases.
Ongoing education and training ensure that healthcare providers maintain proficiency in this critical diagnostic approach. Regular simulation exercises and case reviews help reinforce the systematic application of the H’s and T’s framework.
Conclusion: Mastering the H’s and T’s for Better Outcomes
The H’s and T’s framework provides an essential tool for diagnosing causes of cardiac arrest in the post-ROSC period. By systematically evaluating hypoxia, hypovolemia, hyperkalemia, hypokalemia, hypothermia, tension pneumothorax, tamponade, toxins, and thrombosis, healthcare providers can identify and treat reversible conditions that could otherwise lead to poor outcomes.
Success with this approach requires continuous education, practice, and teamwork. Healthcare providers must remain vigilant for these treatable causes while providing comprehensive post-resuscitation care.
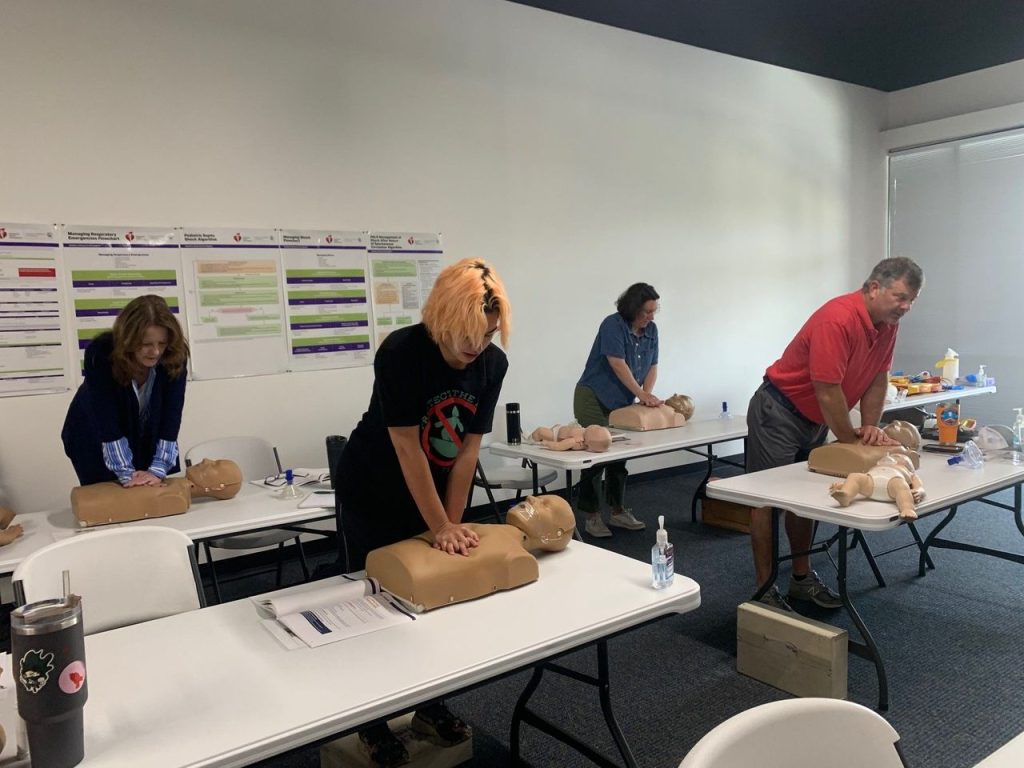
Ready to enhance your emergency response skills? Stay prepared for cardiac emergencies by maintaining current certifications. Whether you need CPR certification Tampa or ACLS certification Tampa, CPR Tampa offers comprehensive training through the American Heart Association. Our stress-free, hands-on courses in BLS for Healthcare Providers, ACLS, PALS, and CPR and First Aid prepare you for real-world emergencies. Choose the best CPR class in Tampa for your certification needs and ensure you’re ready to save lives when it matters most.