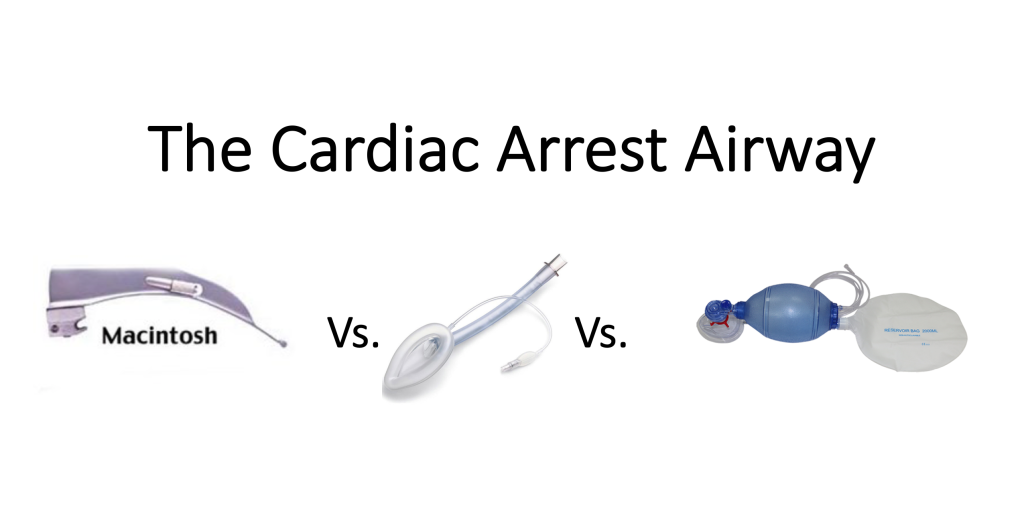
When seconds count during a cardiac arrest or respiratory emergency, having the right airway management skills and devices can make all the difference between life and death. As healthcare providers, understanding the various airway devices available and knowing when to use them is critical for successful resuscitation outcomes. This article explores the differences between basic and advanced airway devices, their applications in emergency care, and why proper training in both is essential for healthcare professionals.
What Are Airway Devices?
Airway devices are specialized medical tools designed to maintain or establish a patent (open) airway in patients who cannot maintain their airway. These devices serve several critical functions during resuscitation:
- Keeping the airway open and clear of obstructions
- Facilitating effective ventilation and oxygenation
- Protecting the lungs from aspiration of stomach contents
- Providing a route for suctioning secretions
- Creating a pathway for delivering positive-pressure ventilation
Airway devices fall into two main categories: basic airway devices and advanced airway devices. Each category serves different purposes and requires varying levels of training and expertise to use effectively during emergencies.
Basic Airway Devices: The First Line of Defense
Basic airway devices are the foundation of airway management and are typically the first tools employed during resuscitation efforts. These devices are relatively simple to use, require minimal training, and can be employed by healthcare providers at various levels, including those with basic life support (BLS) training.
Types of Basic Airway Devices
Oropharyngeal Airways (OPAs)
Oropharyngeal airways, commonly known as oral airways or Guedel airways, are curved plastic devices inserted into the mouth to prevent the tongue from blocking the posterior pharynx. They create a channel for air to flow from the lips to the pharynx.
Key features:
- Available in various sizes for different patients
- Prevent the tongue from obstructing the airway
- Easy to insert with proper technique
- Most suitable for unconscious patients without a gag reflex
Nasopharyngeal Airways (NPAs)
Nasopharyngeal airways, or nasal trumpets, are soft rubber or plastic tubes inserted through the nostril into the posterior pharynx. They provide an air passage from the nares to the pharynx.
Key features:
- Better tolerated in semi-conscious patients with an intact gag reflex
- Available in various sizes based on internal diameter
- Provide a route for suction catheter insertion
- Must be lubricated before insertion to prevent trauma
Bag-Valve-Mask (BVM) Devices
While not strictly an airway device, the BVM is a crucial component of basic airway management, allowing rescuers to deliver positive-pressure ventilation to patients.
Key features:
- Self-inflating bag connected to a face mask
- Can be connected to oxygen to deliver higher concentrations
- Requires a proper seal against the face for effective ventilation
- It can be challenging to use effectively with just one rescuer
Advanced Airway Devices: Enhancing Resuscitation Outcomes
Advanced airway devices provide more definitive airway management, offering better protection against aspiration and more reliable ventilation. These devices typically require advanced training, such as that provided in Advanced Cardiac Life Support (ACLS) certification courses, and more specialized skills to insert correctly.
Types of Advanced Airway Devices
Endotracheal Tubes (ETTs)
Endotracheal intubation involves passing a flexible plastic tube through the vocal cords into the trachea. This is considered the gold standard for securing an airway during resuscitation.
Key features:
- Provides a direct connection to the lungs
- Effectively protects against aspiration
- Allows for suctioning of secretions
- Requires laryngoscopy for visualization during placement
- Enables precise control of ventilation parameters
Supraglottic Airway Devices
Supraglottic airways sit above the glottis (voice box) and provide an alternative to endotracheal intubation that is generally easier to place.
Laryngeal Mask Airways (LMAs):
- Consists of an inflatable mask-like cuff attached to an airway tube
- Create a seal around the laryngeal inlet
- Faster to insert than ETT,s with less training required
- Provide moderate protection against aspiration
- Available in disposable and reusable versions
King Laryngeal Tubes:
- Single-lumen tube with two inflatable cuffs
- Blindly inserted into the esophagus
- Simple to place with minimal training
- Provides adequate ventilation in emergencies
- Often used in pre-hospital settings
i-gel® Airway:
- Made of a gel-like thermoplastic elastomer
- No inflatable cuff, reducing insertion time
- Anatomically designed to fit the pharyngeal and laryngeal structures
- Includes a gastric channel for passing a nasogastric tube
Video Laryngoscopes
These devices incorporate video camera technology to improve visualization of the vocal cords during intubation.
Key features:
- Enhanced view of the glottis without the need to align oral, pharyngeal, and laryngeal axes
- Higher first-attempt success rates, especially in difficult airways
- Require less manipulation of the airway and cervical spine
- Allow for teaching and supervision through a shared view
Differences in CPR with an Advanced Airway
When an advanced airway device is in place during cardiopulmonary resuscitation (CPR), several important modifications to the standard BLS algorithm are necessary.
Ventilation Rate and Timing
Without an advanced airway:
- 30:2 compression-to-ventilation ratio
- Pauses in compressions to deliver breaths
- Coordination is required between rescuers
With an advanced airway:
- Continuous chest compressions without pauses
- Ventilations delivered at a rate of 10 breaths per minute (one breath every 6 seconds)
- No need to synchronize breaths with compressions
Rescuer Roles and Positioning
Without an advanced airway:
- Multiple-rescuer coordination for compressions and ventilations
- Rescuers typically rotate positions to prevent fatigue
With an advanced airway:
- Dedicated provider for ventilation
- Compressors can focus solely on delivering high-quality chest compressions
- More efficient division of tasks among team members
Monitoring and Confirmation
Without an advanced airway:
- Visual chest rise as primary confirmation of effective ventilation
- Limited ability to monitor airway parameters
With an advanced airway:
- Continuous waveform capnography to confirm proper placement and adequate ventilation
- Ability to monitor expired CO2 as an indicator of CPR quality and potential return of spontaneous circulation
Two Main Advantages of Using Advanced Airway Devices
1. Enhanced Protection Against Aspiration
One of the most significant advantages of advanced airway devices, particularly endotracheal tubes, is the protection they provide against aspiration of gastric contents. During cardiac arrest, regurgitation is common due to gastric distension from rescue breathing, decreased lower esophageal sphincter tone, and chest compressions.
Advanced airway devices with cuffs create a seal that prevents stomach contents from entering the lungs. This protection is crucial as aspiration pneumonitis can significantly complicate post-resuscitation care and lead to worse outcomes.
2. More Reliable and Efficient Ventilation
Advanced airway devices allow for more controlled and efficient delivery of ventilation during resuscitation efforts. Benefits include:
- Consistent tidal volumes: Advanced airways enable more precise control over the volume of air delivered with each breath.
- Higher oxygen concentrations: Direct connection to the ventilatory circuit ensures delivery of higher FiO2 (fraction of inspired oxygen).
- Reduced gastric insufflation: By bypassing the upper airway or creating a seal, less air enters the stomach, reducing the risk of vomiting and aspiration.
- Ability to apply PEEP (Positive End-Expiratory Pressure): Advanced airways allow for the application of PEEP, which can improve oxygenation in certain conditions.
- Continuous compressions: As mentioned earlier, advanced airways eliminate the need to pause compressions for ventilation, improving coronary perfusion pressure and resuscitation outcomes.
The Difference Between Basic and Advanced Airway Management
The distinction between basic and advanced airway management extends beyond just the devices used. It encompasses different skill sets, knowledge requirements, and approaches to patient care during resuscitation.
Training and Certification Requirements
Basic airway management:
- Taught in BLS and first aid courses
- Requires minimal specialized equipment
- Can be learned by healthcare providers at all levels
- Focuses on simple techniques like head positioning and basic device insertion
Advanced airway management:
- Taught in ACLS, PALS, and specialized airway management courses
- Requires more extensive training and regular practice
- Typically performed by physicians, advanced practice providers, respiratory therapists, and specially trained paramedics
- Involves understanding the complex anatomy and physiology of the respiratory system
Decision-Making Process
Basic airway management:
- Immediate application in emergency situations
- Simple algorithm-based approaches
- Focus on rapid intervention and basic life support
Advanced airway management:
- Requires assessment of risks vs. benefits
- Consideration of patient-specific factors
- More complex decision trees based on patient presentation
- Often involves medication administration (sedatives, paralytics)
Equipment and Resource Needs
Basic airway management:
- Requires minimal equipment (OPAs, NPAs, BVM)
- Available in most healthcare settings
- Less resource-intensive
Advanced airway management:
- Requires specialized equipment (laryngoscopes, ETTs, video devices)
- May need medication support (sedation, paralysis)
- Often requires additional personnel for optimal placement
- Needs more extensive monitoring capabilities
Choosing the Right Approach: When to Use Basic vs. Advanced Airway Devices
The decision to use basic or advanced airway devices depends on several factors, including:
- Provider skill level and experience: Advanced airways should only be placed by those with proper training and ongoing practice.
- Setting and available resources: Pre-hospital settings may favor simpler devices with fewer complications.
- Patient characteristics: Difficult airways (obesity, short neck, limited mouth opening) may influence device selection.
- Nature and severity of the emergency: Cardiac arrest typically requires more definitive airway management than temporary respiratory distress.
- Expected duration of respiratory support: Longer-term ventilation generally warrants more definitive airway management.
Current resuscitation guidelines emphasize that high-quality chest compressions and basic airway management should take precedence over advanced airway placement, especially if placement would interrupt compressions or if provider experience with advanced techniques is limited.
Best Practices for Airway Management During Resuscitation
Regardless of which airway devices are employed, certain principles apply to all resuscitation scenarios:
- Prioritize oxygenation and ventilation: The primary goal is to ensure adequate oxygen delivery to vital organs.
- Minimize interruptions in chest compressions: When placing any airway device, work around continuous compressions when possible.
- Confirm proper placement: Always verify the correct positioning of any airway device through primary and secondary confirmation methods.
- Have backup plans: Be prepared to switch to an alternative approach if the initial airway management strategy fails.
- Continuous monitoring: Regularly reassess the effectiveness of ventilation and oxygenation throughout the resuscitation effort.
- Team communication: Clear communication about airway status and management plans is essential for coordinated care.
Conclusion: The Importance of Comprehensive Airway Management Training
Both basic and advanced airway devices play crucial roles in resuscitation efforts. While advanced airways offer certain advantages in specific situations, basic airway management skills remain the foundation upon which all emergency airway interventions are built.
Healthcare providers should strive to maintain competency in both basic and advanced airway techniques through regular training, practice, and certification. Understanding the strengths, limitations, and appropriate applications of different airway devices enables providers to deliver optimal care during critical situations.
Take Action: Enhance Your Resuscitation Skills Today
Don’t wait until you’re faced with a respiratory emergency to improve your airway management skills. CPR Classes Tampa offers comprehensive training in both basic and advanced airway management techniques through our American Heart Association-certified courses.
Whether you need BLS for Healthcare Providers certification, ACLS certification in Tampa, or PALS training, our experienced instructors provide stress-free, hands-on learning environments that build confidence and competence. Our CPR certification in Tampa programs ensure you’re prepared to handle any airway emergency with the right knowledge and skills.
Contact CPR Classes Tampa today to schedule your next certification or renewal course and join the ranks of healthcare providers delivering the best possible care during life-threatening emergencies. With our practical approach to resuscitation education, you’ll gain the skills needed to make critical differences in patient outcomes when managing airways during emergencies.