When cardiac arrest strikes, the clock starts ticking. For every minute without intervention, survival chances decrease by 7-10%. This is where Automated External Defibrillators (AEDs) become literal lifesavers. These portable devices, now increasingly available in public spaces, have revolutionized emergency response by enabling rapid defibrillation, often before emergency medical services arrive. This article explores the critical relationship between AED use and Return of Spontaneous Circulation (ROSC) in out-of-hospital settings, highlighting why immediate access to these devices and proper CPR training can dramatically improve survival outcomes.
The Critical Link Between Early Defibrillation and ROSC Rates
Return of Spontaneous Circulation—or ROSC—represents the moment when a heart resumes effective pumping after cardiac arrest. Achieving ROSC is the primary immediate goal of resuscitation efforts, and the speed at which it occurs significantly influences long-term survival and neurological outcomes.
Research consistently demonstrates that early defibrillation is one of the most powerful predictors of achieving ROSC in the field. According to the American Heart Association, when defibrillation is delivered within the first 3-5 minutes of collapse, survival rates can reach 50-70%, compared to less than 5% when defibrillation is delayed beyond 12 minutes.
The science behind this is straightforward but profound. During cardiac arrest, the heart often enters a chaotic rhythm known as ventricular fibrillation (VF) or pulseless ventricular tachycardia (VT). These rhythms prevent effective pumping but can be “reset” by delivering an electrical shock that momentarily stops all cardiac electrical activity, allowing the heart’s natural pacemaker to potentially restart with an organized rhythm.
How AED Technology Enhances CPR Success and ROSC Likelihood
Modern AEDs represent a remarkable intersection of sophisticated technology and user-friendly design. Unlike their hospital counterparts, public-access AEDs are engineered for use by virtually anyone, with or without medical training.
These devices work by:
- Analyzing the heart’s electrical activity through adhesive electrode pads placed on the victim’s chest
- Determining if a shockable rhythm is present
- Delivering the appropriate energy dose when indicated
- Providing voice prompts to guide rescuers through the entire process
What makes AEDs particularly effective in improving ROSC rates is their integration with high-quality CPR. Current devices offer real-time feedback on compression rate, depth, and recoil—critical components that influence blood flow during resuscitation efforts. Many models even include metronomes to help rescuers maintain the optimal compression rate of 100-120 per minute.
The synergy between proper CPR technique and timely defibrillation creates the optimal conditions for ROSC. Chest compressions circulate oxygenated blood to vital organs while building coronary perfusion pressure, which makes the heart more responsive to defibrillation. Meanwhile, defibrillation addresses the underlying electrical problem that triggered the arrest.
Real-World Evidence: ROSC Statistics in AED-Assisted Resuscitations
The empirical data supporting AED implementation is compelling. A comprehensive study published in the New England Journal of Medicine examined over 13,000 out-of-hospital cardiac arrests and found that public-access defibrillation before EMS arrival more than doubled survival rates.
Even more striking are the findings from locations with established AED programs:
- In airports and casinos with strategic AED placement and trained responders, survival rates have exceeded 60%
- Public sports facilities with AED programs report ROSC rates of 71-74% when devices are used within 3 minutes
- Corporate offices with comprehensive AED implementation have demonstrated 40-45% long-term survival for witnessed arrests
These statistics highlight an important reality: the impact of AEDs on ROSC isn’t merely theoretical—it’s consistently demonstrated in real-world settings across diverse environments.
The most successful implementations share common features: strategic device placement, regular maintenance protocols, and integration with broader emergency response systems. When these elements align, achieving ROSC in the field becomes significantly more probable.
Beyond Initial ROSC: How Proper AED Use Affects Long-Term Outcomes
While achieving ROSC represents a crucial first step, the ultimate goal is neurologically intact survival. Here again, AEDs play a vital role by minimizing the duration of cerebral ischemia (inadequate blood flow to the brain).
Studies examining functional outcomes after cardiac arrest consistently show that faster defibrillation correlates strongly with:
- Reduced hospital and ICU length of stay
- Lower incidence of post-resuscitation complications
- Improved neurological function at discharge
- Higher rates of return to the previous quality of life
The relationship appears dose-dependent: for every minute earlier that defibrillation occurs, the likelihood of favorable neurological recovery increases by approximately 7-10%.
This translates to profound real-world implications. Patients who receive prompt AED intervention typically experience shorter recovery periods and better overall outcomes than those who achieve ROSC after prolonged resuscitation efforts. The difference often means returning to work, family, and normal activities rather than requiring long-term care or experiencing significant disability.
Barriers to Optimal AED Utilization and ROSC Improvement
Despite compelling evidence supporting widespread AED implementation, several barriers continue to limit their potential impact on ROSC rates:
- Availability gaps: Many high-risk locations still lack accessible AEDs
- Public awareness challenges: Studies show that fewer than 50% of bystanders can identify an AED, and even fewer feel confident using one
- Maintenance issues: Between 10-23% of deployed AEDs have been found to have maintenance problems that could affect performance
- Integration difficulties: AEDs sometimes exist in isolation rather than as part of comprehensive emergency response systems
Addressing these challenges requires multifaceted approaches, including legislation supporting public access defibrillation, community education initiatives, and systematic maintenance programs.
Organizations that successfully overcome these barriers typically see significant improvements in ROSC rates and overall cardiac arrest outcomes.
Combining CPR and AED Use: The Optimal Approach for Field ROSC
The most effective approach to achieving ROSC in the field involves the seamless integration of high-quality CPR with timely defibrillation. This combination, often called the “Chain of Survival,” maximizes the chances of successful resuscitation.
Current guidelines emphasize:
- Immediate recognition and activation of emergency response
- Early CPR with emphasis on chest compressions
- Rapid defibrillation via AED
- Advanced life support and post-resuscitation care
The interplay between these elements is critical. CPR maintains minimal organ perfusion and “primes” the heart for defibrillation, while defibrillation addresses the underlying electrical disturbance. Neither intervention alone is as effective as their coordinated application.
Training programs that teach both skills together, rather than as separate modules, typically produce rescuers who achieve higher ROSC rates in real-world scenarios. This integrated approach recognizes that the physiological processes supporting successful resuscitation require both mechanical (CPR) and electrical (defibrillation) interventions working in concert.
Community Implementation: Models That Maximize ROSC Through Strategic AED Deployment
Communities that have achieved the highest ROSC rates have moved beyond simply placing AEDs in public spaces to developing comprehensive systems of care. These successful models typically include:
- Strategic placement analysis: Using geographic and demographic data to position AEDs where they’re most likely to be needed
- Integrated notification systems: Technologies that alert nearby trained responders when an AED is needed
- Widespread training initiatives: Programs ensuring a critical mass of community members are prepared to perform CPR and use AEDs
- Regular maintenance protocols: Systematic checks ensuring devices remain functional
- Data collection and quality improvement: Tracking outcomes to continuously refine implementation strategies
Cities like Seattle, Copenhagen, and Amsterdam have pioneered such approaches, achieving ROSC rates significantly above national averages. Their success demonstrates that thoughtful implementation can substantially improve outcomes beyond what would be expected from AED placement alone.
The most effective programs recognize that technology, training, and systems design must work together to maximize ROSC rates and save lives.
Future Directions: Emerging Technologies Enhancing Field ROSC Rates
The landscape of resuscitation technology continues to evolve, with several innovations showing promise for further improving ROSC rates:
- Smart AEDs with enhanced rhythm analysis capabilities and automated CPR feedback
- Mobile AED delivery via drones in areas where rapid ground transport is challenging
- Wearable defibrillators for high-risk patients awaiting permanent device implantation
- Smartphone applications that locate nearby AEDs and provide real-time guidance to bystanders
- Telemedicine integration allows for remote medical oversight during resuscitation attempts
These technologies aim to address remaining gaps in the chain of survival, particularly in challenging environments or for vulnerable populations. Early research suggests they may further improve the already significant impact of standard AEDs on ROSC rates.
As these innovations move from research to implementation, the potential for achieving field ROSC—even in previously challenging scenarios—continues to grow.
Conclusion: The Undeniable Impact of AEDs on Field ROSC Rates
The evidence is clear: when properly implemented and used, AEDs dramatically improve the likelihood of achieving ROSC in out-of-hospital cardiac arrests. Their impact extends beyond immediate survival to influence long-term outcomes and quality of life for survivors.
As public access defibrillation programs continue to expand, more lives will be saved through this remarkable technology. However, the full potential of AEDs can only be realized when they’re part of comprehensive systems including widespread CPR training, strategic deployment, proper maintenance, and continuous quality improvement.
The time-sensitive nature of cardiac arrest means that communities cannot afford to delay implementing robust AED programs. Every minute saved in delivering defibrillation translates directly to lives saved and neurological function preserved.
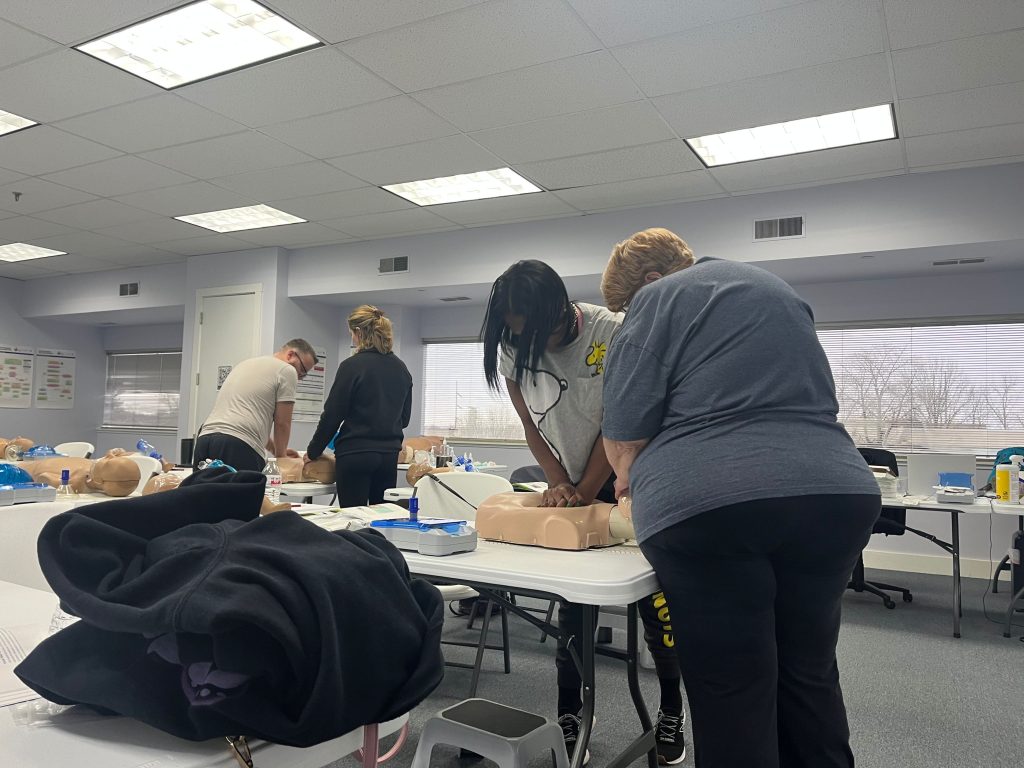
Take Action: Be Prepared with CPR and AED Training
Don’t wait for an emergency to learn these critical skills. CPR Cincinnati, an American Heart Association training site, offers comprehensive certification and renewal courses in BLS for Healthcare Providers, ACLS, PALS, and CPR and First Aid. Their stress-free, hands-on classes ensure you’ll be confident and prepared to respond effectively in an emergency.
Whether you’re a healthcare professional seeking BLS certification in Cincinnati or a community member wanting to learn basic CPR, CPR Cincinnati provides the highest quality training available. Their experienced instructors make learning these life-saving skills accessible to everyone.
Visit CPR Cincinnati today to schedule your CPR certification in Cincinnati and join the community of prepared responders who can make the difference between life and death when minutes matter.