When managing cardiac arrest, healthcare providers must quickly identify and address potential underlying causes. The American Heart Association has organized these causes into two memorable categories: the 5 Hs and the 5 Ts. These serve as a crucial framework for assessment and intervention during resuscitation efforts.
Hypoxia: The Critical Need for Oxygen
Hypoxia, or insufficient oxygen supply to body tissues, represents one of the most common and dangerous conditions in cardiac emergencies. When cells don’t receive adequate oxygen, they begin to fail, potentially triggering or worsening cardiac arrest. Healthcare providers must recognize that hypoxia can result from various conditions, including respiratory failure, severe asthma, or pulmonary edema.
Early recognition of hypoxia involves assessing for signs such as cyanosis, shortness of breath, and altered mental status. Treatment typically begins with immediate oxygen supplementation and addressing the underlying cause. In many cases, proper airway management becomes essential, potentially requiring intubation or other advanced airway interventions.
Hypovolemia: Understanding Volume Depletion
Hypovolemia occurs when the body loses a significant amount of blood or fluids, leading to inadequate circulation. This condition can result from severe bleeding, dehydration, or extensive burns. The heart cannot function effectively without adequate blood volume, potentially leading to cardiac arrest.
Healthcare providers must assess for signs of hypovolemia, including:
- Decreased blood pressure
- Rapid, weak pulse
- Cool, clammy skin
- Delayed capillary refill
- Altered mental status
Treatment focuses on rapid volume replacement through intravenous fluids or blood products, depending on the cause and severity of the volume loss.
Hydrogen Ion (Acidosis): The pH Balance Challenge
Acidosis, an excess of hydrogen ions in the body, can severely impact cardiac function. This condition may develop from various situations, including prolonged cardiac arrest, severe infection, or diabetic complications. The heart’s ability to contract effectively diminishes as the blood becomes more acidic.
Healthcare providers must consider both respiratory and metabolic causes of acidosis. Treatment approaches vary based on the underlying cause but may include:
- Ventilatory support to address respiratory acidosis
- Sodium bicarbonate administration in severe cases
- Addressing the primary condition causing the acid-base imbalance
Hyperkalemia/Hypokalemia: The Potassium Problem
Potassium imbalances, whether elevated (hyperkalemia) or diminished (hypokalemia), can greatly affect cardiac function. These electrolyte disturbances frequently present with distinct ECG changes and may lead to life-threatening arrhythmias.
Management strategies differ based on whether potassium levels are elevated or decreased:
For hyperkalemia:
- Calcium administration to stabilize cardiac membranes
- Insulin with glucose to shift potassium intracellularly
- Sodium bicarbonate in acidotic patients
- Emergency dialysis in severe cases
For hypokalemia:
- Careful potassium replacement
- Monitoring for associated magnesium deficiency
- Addressing underlying causes such as diuretic use
Hypothermia: Temperature Management Matters
Hypothermia, defined as a core body temperature below 95°F (35°C), can cause significant cardiac dysfunction. This condition may result from environmental exposure, immersion incidents, or even therapeutic interventions.
Treatment approaches must be systematic and may include:
- Active external warming measures
- Warm intravenous fluids
- Modified resuscitation protocols for severely hypothermic patients
- Prevention of further heat loss
Tension Pneumothorax: The Pressure Problem
A tension pneumothorax develops when air enters the pleural space but cannot escape, creating increasing pressure that compromises cardiac function. This condition requires immediate recognition and intervention.
Key clinical features include:
- Absent breath sounds on the affected side
- Tracheal deviation away from the affected side
- Distended neck veins
- Rapidly deteriorating vital signs
Emergency needle decompression or chest tube placement becomes necessary to relieve the pressure and restore normal cardiac function.
Tamponade: Understanding Cardiac Compression
Cardiac tamponade occurs when fluid accumulates in the pericardial space, compressing the heart and preventing proper filling. This condition can rapidly lead to cardiac arrest if not promptly identified and treated.
Healthcare providers should watch for the classic signs:
- Beck’s triad (hypotension, muffled heart sounds, distended neck veins)
- Pulsus paradoxus
- Electrical alternans on ECG
Emergency pericardiocentesis may be necessary to relieve the tamponade and restore cardiac function.
Toxins: The Chemical Culprits
Toxins encompass a wide range of substances that can cause or contribute to cardiac arrest. These may include prescription medications, illegal drugs, or environmental toxins.
Management typically involves:
- Identifying the specific toxin when possible
- Administering appropriate antidotes
- Supporting vital functions
- Preventing further absorption
- Enhancing the elimination of the toxin
Thrombosis: Pulmonary and Coronary Concerns
Thrombosis in either the pulmonary or coronary vessels can precipitate cardiac arrest. Pulmonary embolism and acute coronary syndrome represent the two main categories of concern.
Treatment approaches may include:
- Fibrinolytic therapy in appropriate candidates
- Anticoagulation
- Mechanical intervention when indicated
- Supportive care measures
Taking Action: Enhancing Your Resuscitation Skills
Understanding the 5 Hs and Ts is crucial for healthcare providers, but knowledge alone isn’t enough. Regular training and certification ensure you’re prepared to put this knowledge into practice effectively.
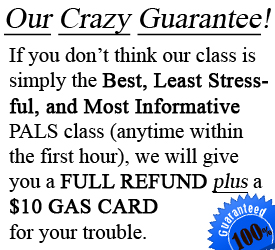
If you’re in the Tampa area, CPR Tampa offers comprehensive training programs that cover these critical concepts and more. As an American Heart Association training site, we provide:
- Stress-free, hands-on learning environments
- Initial certifications and renewals
- BLS for Healthcare Providers
- ACLS certification
- PALS certification
- CPR and First Aid courses
For healthcare providers in Tampa seeking to enhance their resuscitation skills, we recommend pursuing CPR certification in Tampa and ACLS certification in Tampa through authorized American Heart Association training centers.
Remember, in cardiac arrest situations, quick identification and treatment of underlying causes can mean the difference between life and death. Stay current with your certifications and maintain your knowledge of the 5 Hs and Ts to provide the best possible care for your patients.
Contact CPR Tampa today to schedule your certification or renewal course. Our experienced instructors will ensure you’re well-prepared to handle any cardiac emergency with confidence and competence.