When it comes to administering first aid, the protocols for children can differ significantly from those for adults. A child’s smaller size, developing physiology, and distinct emotional needs require specialized approaches to ensure their safety and well-being. As medical professionals, it is crucial to understand and apply these pediatric-specific techniques to provide effective care in emergencies.
CPR Techniques for Children
Cardiopulmonary resuscitation (CPR) is a life-saving procedure that can be the difference between life and death in cardiac and respiratory emergencies. However, the techniques used for children vary from those used for adults due to their smaller body size and physiological differences.
A. Chest Compression Depth and Rate
For children aged 1 to puberty, chest compressions should be delivered at a depth of at least one-third the anterior-posterior diameter of the chest, or approximately 2 inches (5 cm). The rate of compressions should be 100-120 per minute, allowing for complete chest recoil between each compression. In contrast, for adults, the recommended compression depth is at least 2 inches (5 cm), but no more than 2.4 inches (6 cm). The rate remains the same at 100-120 compressions per minute.
B. Rescue Breathing Techniques
When providing rescue breaths to a child, the head-tilt/chin-lift technique should be used to open the airway. Pinch the child’s nose closed and deliver two slow breaths, each lasting 1 second, making sure the chest rises with each breath. For infants (under 1 year old), the head-tilt/chin-lift may need to be modified to avoid excessive airway obstruction. Use a mouth-to-mouth-and-nose technique, covering both the infant’s mouth and nose with your mouth.
C. AED Use and Pad Placement
Automated external defibrillators (AEDs) can be used on children over 1 year old, but special pediatric pads or dosages may be required, depending on the device. If pediatric pads are unavailable, adult pads can be used, positioning them according to the child’s size and following the AED’s prompts. Proper CPR techniques tailored to a child’s age and size are critical for increasing their chances of survival in a cardiac or respiratory emergency. Medical professionals must stay up-to-date on pediatric CPR protocols and be prepared to adapt their approach accordingly.
Choking Management
Choking is one of the leading causes of unintentional injury and death in children, making prompt recognition and treatment essential. The approach to managing a choking incident differs for children compared to adults due to their smaller airway size and varying levels of consciousness.
A. Conscious vs Unconscious Protocol
If a child is coughing, wheezing, or able to speak, allow them to continue coughing and clearing their airway on their own. Do not perform any intervention unless the child becomes unconscious or unable to cough, cry, or breathe effectively. For a conscious choking child over 1-year-old, give back blows followed by abdominal thrusts until the object is dislodged or the child becomes unconscious. If the child becomes unconscious, immediately begin CPR, starting with chest compressions. Look inside the mouth and remove any visible object before attempting rescue breaths.
B. Back Blows and Abdominal Thrusts
To give back blows, place the child in a forward-leaning position and firmly strike between the shoulder blades with the heel of your hand. For abdominal thrusts on a child over 1 year old, stand or kneel behind them, making a fist and placing it just above the navel. Cover your fist with your other hand and give inward and upward thrusts until the object is dislodged. For infants under 1-year-old, give back blows and chest thrusts rather than abdominal thrusts to avoid potential injury.
C. Adjustments Based on Child’s Size/Age
The techniques used should be adjusted based on the child’s size and age. For example, abdominal thrusts may need to be delivered with less force on smaller children to prevent internal injury. Always call emergency services if a choking incident occurs. Prompt recognition of choking signs and proper protocols are crucial when a child’s airway is obstructed. Medical professionals must be prepared to act swiftly and adapt their approach to the child’s age and size.
Wound Care
Treating wounds in children requires specific considerations to prevent further injury and promote proper healing. From controlling bleeding to cleaning and dressing wounds, pediatric protocols differ from those used for adults.
A. Controlling Bleeding
Apply firm, direct pressure using a clean dressing or cloth to control bleeding from a wound. For severe bleeding, use a tourniquet if bleeding doesn’t stop in 10 minutes call 911 immediately. Tourniquets should only be used as a last resort for life-threatening bleeding in children. Elevate the injured area above the level of the heart if possible to help reduce bleeding and swelling. Do not remove any embedded objects as this could cause further bleeding.
B. Cleaning and Dressing Wounds
Gently clean the wound area with mild soap and water to remove dirt and debris. Avoid using hydrogen peroxide or iodine, which can damage fragile skin tissue. Cover the cleaned wound with an antibiotic ointment and sterile bandage appropriate for the child’s size. Reinforce dressings with tape or roller gauze if needed to keep them securely in place.
C. Pediatric Trauma Considerations
Children’s bones are smaller and softer than adults’, so extra care is needed when immobilizing fractures using splints or slings. Apply just enough pressure to stabilize without restricting blood flow. For head injuries, monitor the child closely for signs of concussion such as vomiting, dizziness, or abnormal behavior. Seek immediate medical attention if symptoms worsen or don’t improve. Proper wound cleaning, dressing, and immobilization techniques specific to pediatric patients help minimize further harm and promote optimal healing. Medical professionals must exercise vigilance when treating traumatic injuries in children.
Environmental Emergencies
Children are especially vulnerable to the effects of extreme temperatures and environmental exposures due to their smaller body mass and surface area. Prompt recognition and treatment of conditions like hypothermia, heat illness, and bites/stings is crucial.
A. Hypothermia/Frostbite
If a child shows signs of hypothermia such as shivering, lethargy, or confusion, immediately move them to a warm, dry area. Remove any wet clothing and cover them with blankets. Give them warm, sweet drinks if they are alert. For mild frostbite (redness/pain in extremities), rewarm the affected area with body heat. Do not rub or massage the skin. For severe frostbite with white/blue skin, cover with sterile dressings and get emergency medical care.
B. Heat Exhaustion/Heatstroke
Move the child to a cool, shaded area and have them lie down with their feet elevated. Loosen clothing and apply cool, wet clothes to their body, especially the groin, armpits, and neck. Give small sips of cool water and monitor for signs of heatstroke such as hot, flushed skin, rapid pulse, nausea/vomiting, or altered mental status. Immediately call 911 if heatstroke is suspected.
C. Bites/Stings
For minor bites or stings, wash the area with soap and water and apply a cold pack to reduce swelling and pain. Watch for signs of allergic reaction. For severe reactions with swelling, difficulty breathing, dizziness, or nausea, call 911 immediately. Assist with the child’s epinephrine auto-injector if they have one. Children have an increased risk of hypothermia, heat illness, and severe reactions from bites/stings. Knowledge of environment-specific first aid allows medical professionals to swiftly recognize and treat these emergencies when they occur.
Medication Administration
Ensuring the proper dosage and administration of medications is critical when treating pediatric patients. Miscalculations or improper techniques can have serious consequences for a child’s health and safety.
A. Proper Dosing Calculations
Medication dosages for children are typically based on weight rather than age alone. Always verify the child’s current weight and consult age-appropriate dosing guidelines. Pay close attention to units of measurement, as dosages are often measured in milliliters or milligrams rather than teaspoons or tablets formulated for adults. Double-check all dosage calculations, especially for high-risk medications like anticoagulants or chemotherapies, to avoid dangerous over- or under-dosing errors.
B. Intake Routes
The Route of administration may need to be modified for pediatric patients. Oral liquids or dissolving tablets are often preferred over capsules or tablets that can be difficult for children to swallow. Subcutaneous or intramuscular injections require precise technique and needle length/gauge selection based on the child’s age and body habitus. Inhaled medications administered via metered-dose inhalers or nebulizers may require spacers or masks designed specifically for pediatric use.
C. Avoiding Medication Errors
Label all medications clearly, including the child’s name, drug name, dosage, route, and time of administration. Verify allergies and medications with parents/caregivers. Have a second medical professional independently verify all high-risk medication dosage calculations before administration. Document all medications given, the time administered, dose, route, and the child’s response. Paying close attention to weight-based dosing, administration routes, and double-checking processes can significantly reduce the risk of potentially dangerous medication errors in pediatric patients. Medical professionals must maintain vigilance when administering any drug to children.
Conclusion
Providing effective first aid and emergency care to pediatric patients requires specialized knowledge and techniques tailored to their unique physiology and needs. From CPR to wound care, medication administration to environmental exposures, the protocols for treating children can differ significantly from those used for adults.
As medical professionals, it is our responsibility to stay up-to-date on pediatric-specific first-aid protocols through regular training and certification renewals. Maintaining these vital skills ensures we can respond appropriately and confidently when a child’s life hangs in the balance. CPR St. Louis offers comprehensive CPR certification courses covering pediatric emergency response.
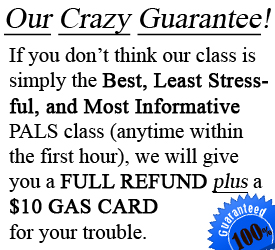
CPR St. Louis is an American Heart Association training site that provides initial CPR certification in St. Louis as well as renewals for BLS, ACLS, and PALS. Their hands-on, stress-free classes equip medical providers with the latest pediatric emergency protocols. Enroll in an upcoming CPR certification St. Louis course to master pediatric first aid and CPR techniques.
With proper training from respected programs like those offered by CPR St. Louis, medical professionals can provide children with the high-quality, age-appropriate care they need during emergencies. Remaining vigilant, following best practices, and continuing to expand our pediatric knowledge through regular certification is essential to safeguarding the health and well-being of our youngest patients.